LIBRE Profile
LIBRE Profile is an innovative system for measuring a return to life after burn injury.
Attempting to return to everyday life after a burn injury can be difficult, stressful, and emotionally challenging. While traditional rehabilitation strategies for burn survivors focus on physical recovery, Life Impact Burn Recovery Evaluation (LIBRE) Project focuses on the impact burn injuries have on social life.
LIBRE Profile is a computer-based questionnaire that can help burn survivors and clinicians track burn recovery, improve rehabilitation efforts, and identify areas where additional support is needed.

LIBRE Journey Study
The LIBRE Journey Study is developing social recovery trajectories using the LIBRE Profile questionnaire. These trajectories are similar to growth curves for kids and they will help burn survivors and their clinicians understand LIBRE Profile scores.
The LIBRE Journey Study aims to create social recovery trajectories for the LIBRE Profile questionnaire. Social recovery trajectories are similar to growth curves for kids and they allow social integration to be assessed over time. On a clinical level, established trajectories will promote resource planning and development, identify clinical care needs, and foster design and assessment of targeted interventions. They will also help burn survivors understand their LIBRE Profile scores and see how they are doing with social integration in comparison to others with a similar injury.
In this study, the LIBRE Profile will be administered at five time points over a 2 year period. Participants will be compensated with an Amazon gift card up to $100 in value.
Participants must be:
- Over the age of 18; and
- Have burns to ≥5% of their body or to hands, face, feet or genitalia.
If you are interested in participating, please contact us at:
BostonHarvardBIMS@partners.org



Preschool & School-Aged LIBRE Study
The Preschool and School-Aged LIBRE Study are developing a computer-based questionnaire to assess the impact of burn injury on child health. These studies will evaluate different health outcomes related to children’s physical and social recovery after a burn injury.
Dr. Colleen Ryan is currently researching burn injury outcomes in children up to the age of 12 through two studies: Preschool LIBRE and School-Aged LIBRE.
Both studies are developing a computer-based questionnaire to assess the impact of burn injury on child health. The Preschool LIBRE (1-5 years) and School-Aged LIBRE (5-12 years) will evaluate outcomes related to key aspects of child health and functioning such as physical, social, psychological, and family functioning. Once developed, the questionnaire will be used by parents of children with burns and their clinicians to track recovery and help improve rehabilitation and early intervention efforts.
Both studies are actively enrolling parents or legal guardians of children aged 1-12 with burn injuries. Participants will be compensated with a $15 e-gift card for their time.
In this study, the LIBRE Profile will be administered at five time points over a 2 year period. Participants will be compensated with an Amazon gift card up to $100 in value.
For more information or to enroll please contact:
Children aged 1-5 years:
Children aged 5-12 years:
The LIBRE Profile: Assessing Burn Survivors' Social Participation
The video describes why and how we created the LIBRE Profile, as well as how it will be used once it’s ready to be distributed to the burn community. Watch this short video, we hope you enjoy it!
Burn Model Systems National Longitudinal Database
BHBIMS is dedicated to contributing to the Burn Model Systems (BMS) National Database, a prospective, longitudinal, multicenter research study that examines functional and psychosocial outcomes following burns. The BMS National Database consists of data collected from almost 4,000 adults and over 2,000 children with moderate to severe burn injury. In collaboration with the three other NIDILRR-funded BMS sites, we aim to conduct rigorous long-term research that:
- Leads to improved care and outcomes of individuals with severe burn injuries.
- Contributes to evidence-based rehabilitation interventions and clinical practice guidelines for persons with severe burns.
- Studies the longitudinal course and secondary effects of severe burn injuries.
- Identifies and evaluates trends over time.
- Establishes expected rehabilitation outcomes for burn survivors.
- Facilitates other projects, including clinical trials and population-based studies.
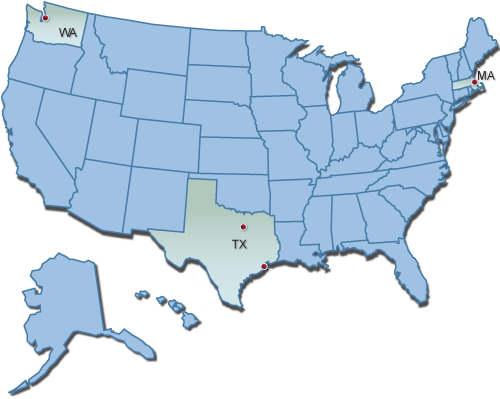
The other three BMS centers:
- Northwest Regional Burn Model System: Seattle, Washington
- Pediatric Burn Injury Rehabilitation Model System: Galveston, Texas
- North Texas Burn Rehabilitation Model System: Dallas, Texas
We welcome the use of the BMS National Database by external researchers who share our goal of improving the lives of burn survivors. Please click here for details.
Visit the Burn Model System Data and Statistical Center website for more information.
To learn more, see our 2021 BMS National Database Facts and Figures:
Publications
J Burn Care Res. 2024 Jun 29:irae134. doi: 10.1093/jbcr/irae134. Online ahead of print.
ABSTRACT
Burn survivors can experience social participation challenges throughout their recovery. The aim of this study was to develop a novel Australian English translation of the Life Impact Burn Recovery Evaluation (LIBRE) Profile, the Aus-LIBRE Profile. This study consisted of three stages: 1) translation of the LIBRE Profile from American to Australian English by Australian researchers/burns clinicians; 2) piloting and cognitive evaluation of the Aus-LIBRE Profile with burn survivors to assess the clarity and consistency of the interpretation of each individual item, and 3) review of the Aus-LIBRE Profile by colleagues who identify as Aboriginal Australians for cross-cultural validation. In stage 2, investigators administered the translated questionnaire to 20 Australian patients with burn injuries in the outpatient clinic (10 patients from xx and 10 patients from yy). Face validity of the Aus-LIBRE Profile was tested in 20 burns survivors (11 females) ranging from 21 to 74 years (median age 43 years). The total body surface area (TBSA) burned ranged from 1% to 50% (median 10%). Twelve language changes were made based on the feedback from the burn clinicians/researchers, study participants and colleagues who identify as Aboriginal Australians. Using a formal translation process, the Aus-LIBRE Profile was adapted for use in the Australian burn population. The Aus-LIBRE Profile will require psychometric validation and testing in the Australian burn patient population before broader application of the scale.
PMID:38943673 | DOI:10.1093/jbcr/irae134
J Burn Care Res. 2024 Jun 29:irae129. doi: 10.1093/jbcr/irae129. Online ahead of print.
ABSTRACT
Burn reconstruction outcomes are an area of growing investigation. Although there is evidence of measured physical improvements in scar characteristics after laser treatment, there is little information on patient reported outcomes. The purpose of this study is to compare patient reported outcomes between burn survivors with and without laser treatment. The study included participants in the Burn Model Systems National Database at a single center; participants that received outpatient laser treatment for burn scars were compared to a matched group of burn survivors that did not receive laser. The following outcomes were examined: Satisfaction With Life Scale, Mental and Physical Component Summary of the Veterans Rand Survey, and the PROMIS Pain Intensity Scale. Regression analyses examined the associations between laser treatment and each outcome at 12 and 24 months. The study population included 287 adult burn survivors (65 laser group, 222 control group). The significant differences found between the two groups included: burn size (laser: 14.9, 13.5 SD, control: 8.9, 11.1 SD; p<0.001), insurance type (p=0.036), inhalation injury (laser: 17.2%, control: 2.7%; p<0.001), and ventilator requirement (laser: 27.7%, control: 13.5%; p=0.013). Laser treatment was not associated with any of the outcomes at both follow-up time points. Further research is needed to develop patient reported outcome measures that are more sensitive to the clinical changes experienced by burn survivors receiving laser treatment.
PMID:38943510 | DOI:10.1093/jbcr/irae129
Burns. 2024 Jun 17:S0305-4179(24)00188-8. doi: 10.1016/j.burns.2024.06.003. Online ahead of print.
ABSTRACT
INTRODUCTION: An area of rehabilitation research in burns is the impact of co-morbidities on disease trajectory. Obesity is a comorbidity of increasing public health concern, but its role remains controversial regarding burn injury and physical recovery. Our aim was to evaluate the association between body mass index (BMI) categories as a measure of obesity at discharge and self-reported physical function (PF) during recovery of adult burn survivors.
METHODS: This is a retrospective study on data collected by four major US burn centers, which contribute to the Burn Model System National Database. The data included BMI obtained at hospital discharge and self-reported PF-mobility, using the PROMIS measures assessed at 6, 12, and 24 months after burn. Subjects were classified into weight status categories based on BMI: underweight (BMI <18.5), normal weight (18.5 ≤ BMI <25), overweight (25 ≤ BMI <30), obesity class 1 (30 ≤ BMI <35), obesity class 2 (35 ≤ BMI <40), and obesity class 3 (BMI ≥40). Mixed-effects linear regression models were used to assess the association between BMI categories and PF scores over time, adjusted for patient and injury characteristics.
RESULTS: A total of 496 adult burn patients aged 47 ± 16 years were included, with mean total body surface area (TBSA) burned of 18 ± 19 % and mean BMI at discharge of 28 ± 7 kg/m2. PROMIS PF scores significantly improved over time in the recovery phase after burn (time effect, p < 0.001). Compared to overweight burn patients, normal-underweights exhibited lower PF score by an average of 4.06 units (p = 0.001) but scores increased linearly by an estimated 0.17 units per month (p = 0.01) over the 24 months after discharge. Similarly, compared to overweight burn patients, class 1 obese reported lower PF score by a mean 2.67 units (p = 0.07) but PF increased linearly by 0.15 units per month (p = 0.07) over the 24 months after discharge. These findings were independent of the effects of age at discharge, sex, TBSA burned, and hand and leg burn.
CONCLUSION: Being overweight was associated with improved and faster recovery of PF scores compared to normal, underweight, and obese burn patients during long-term recovery. Hence, our data suggests that long-term recovery and restoration of PF in adult burn survivors is not compromised by a small excess in body weight.
PMID:38918151 | DOI:10.1016/j.burns.2024.06.003
Arch Phys Med Rehabil. 2024 May 14:S0003-9993(24)01000-1. doi: 10.1016/j.apmr.2024.05.011. Online ahead of print.
ABSTRACT
OBJECTIVE: To examine the moderation effects of daily behavior on the associations between symptoms and social participation outcomes after burn injury.
DESIGN: A 6-month prospective cohort study.
SETTING: Community.
PARTICIPANTS: Twenty-four adult burn survivors.
INTERVENTIONS: Not applicable.
MAIN OUTCOME MEASURES: Symptoms and social participation outcomes were assessed weekly using smartphone surveys, including symptoms of pain (Patient-Reported Outcomes Measurement Information System [PROMIS] Pain Intensity and Pain Interference), anxiety (PROMIS Anxiety), and depression (Patient Health Questionnaire), as well as outcomes of social interactions and social activities (Life Impact Burn Recovery Evaluation [LIBRE] Social Interactions and Social Activities). Daily behaviors were automatically recorded by a smartphone application and smartphone logs, including physical activity (steps, travel miles, and activity minutes), sleep (sleep hours), and social contact (number of phone calls and message contacts).
RESULTS: Multilevel models controlling for demographic and burn injury variables examined the associations between symptoms and social participation outcomes and the moderation effects of daily behaviors. Lower (worse) LIBRE Social Interactions and LIBRE Social Activities scores were significantly associated with higher (worse) PROMIS Pain Intensity, PROMIS Pain Interference, PROMIS Anxiety, and Patient Health Questionnaire-8 scores (P<.05). Additionally, daily steps and activity minutes were associated with LIBRE Social Interactions and LIBRE Social Activities (P<.05), and significantly moderated the association between PROMIS Anxiety and LIBRE Social Activities (P<.001).
CONCLUSIONS: Social participation outcomes are associated with pain, anxiety, and depression symptoms after burn injury, and are buffered by daily physical activity. Future intervention studies should examine physical activity promotion to improve social recovery after burns.
PMID:38754720 | DOI:10.1016/j.apmr.2024.05.011
J Trauma Acute Care Surg. 2024 May 9. doi: 10.1097/TA.0000000000004384. Online ahead of print.
ABSTRACT
Trauma centers demonstrate an impressive ability to save lives, as reflected by inpatient survival rates of over 95% in the United States. Nevertheless, we fail to allocate sufficient effort and resources to ensure that survivors and their families receive the necessary care and support after leaving the trauma center. The objective of this scoping review is to systematically map the research on collaborative care models (CCM) that have been put forward to improve trauma survivorship. Of 833 articles screened, we included 16 studies evaluating eight collaborative care programs, predominantly in the U.S. The majority of the programs offered care coordination and averaged 9-months in duration. Three-fourths of the programs incorporated a mental health provider within their primary team. Observed outcomes were diverse: some models showed increased engagement (e.g., Center for Trauma Survivorship, trauma quality-of-life follow-up clinic), while others presented mixed mental health outcomes and varied results on pain and healthcare utilization. The findings of this study indicate that collaborative interventions may be effective in mental health screening, PTSD and depression management, effective referrals, and improving patient satisfaction with care. A consensus on core elements and cost-effectiveness of CCMs is necessary to set the standard for comprehensive care in post-trauma recovery.
PMID:38720203 | DOI:10.1097/TA.0000000000004384
Am J Phys Med Rehabil. 2024 Apr 30. doi: 10.1097/PHM.0000000000002512. Online ahead of print.
ABSTRACT
OBJECTIVE: Pain is common in inpatient rehabilitation patients; however, the prevalence of pain diagnoses in this population is not well-defined. This study examines comorbid pain diagnoses in inpatient rehabilitation patients across impairment groups.
DESIGN: Adult inpatient rehabilitation patients discharged from January 2016 through December 2019 were identified in the Uniform Data System for Medical Rehabilitation® database using a literature-established framework containing ICD-10-CM pain diagnoses. Demographic data, clinical data, and pain diagnoses were compared across the 17 rehabilitation impairment groups.
RESULTS: Of 1,925,002 patients identified, 1,347,239 (70.0%) had at least one ICD-10 pain diagnosis. Over half of all patients in each impairment group had at least one pain diagnosis. The most common pain diagnoses were limb/extremity and joint pain, with variation between impairment groups. Female sex and being in the arthritis, major multiple trauma, and pain syndrome impairment groups were associated with a greater odds of a pain diagnosis.
CONCLUSION: Over half of all patients in each rehabilitation impairment group have a pain diagnosis, which varies between impairment groups. Due to the high prevalence of pain diagnoses, a new focus on pain management in inpatient rehabilitation patients is needed. Rehabilitation outcomes may also be affected by pain.
PMID:38709650 | DOI:10.1097/PHM.0000000000002512
Cureus. 2024 Feb 12;16(2):e54079. doi: 10.7759/cureus.54079. eCollection 2024 Feb.
ABSTRACT
Patients with a history of blood clots are commonly placed on anticoagulation therapy, but a common adverse effect of this therapy is hemorrhage. Our patient with a history of left ventricle thrombus in a free-standing inpatient rehabilitation hospital had ecchymoses that expanded over a large portion of the posterior thigh in one day. The rapid expansion of the ecchymoses coupled with a decline in hemoglobin levels prompted an immediate evaluation that showed an intramuscular hematoma. With hemoglobin levels dropping significantly, the patient was then transferred to the emergency department for higher levels of care. A multidisciplinary team of vascular surgery and electrophysiology physicians decided to discontinue anticoagulation and monitor the hematoma with serial compartment checks. The hematoma had stabilized throughout the hospital stay without surgical intervention. This case will discuss the difficulty of managing a patient with a history of previous blood clots with an adductor magnus hematoma in the setting of concurrent iatrogenic anticoagulation. Furthermore, we will review the current management and evaluation of intramuscular hematomas.
PMID:38481892 | PMC:PMC10937031 | DOI:10.7759/cureus.54079
Burns. 2024 May;50(4):957-965. doi: 10.1016/j.burns.2024.01.017. Epub 2024 Jan 19.
ABSTRACT
INTRODUCTION: Heterotopic ossification (HO), or ectopic bone formation in soft tissue, is a not so rare and poorly understood debilitating sequela of burn injury. Individuals developing HO following burn injuries to their hands often experience reductions in mobility, significant contractures, and joint pain. This study identifies demographic characteristics of individuals who develop HO and compares their physical and psychosocial outcomes to the general burn population.
METHODS: Participant demographics, injury characteristics, and PROMIS-29 scores across three time points (discharge, six- and 12- months after injury) were extracted from the Burn Model System National Longitudinal Database representing participants from 2015-2022. Mixed-effects linear regression models were used to compare PROMIS scores across all three longitudinal measurements. Models were adjusted for age, sex, race/ethnicity, HO status, and burn size.
RESULTS: Of the 861 participants with data concerning HO, 33 were diagnosed with HO (3.8% of participants). Most participants with HO were male (n = 24, 73%) and had an average age of 40 + /- 13 years. Participants with HO had significantly larger burn size (49 +/-23% Total Body Surface Area (TBSA)) than those without HO (16 +/-17%). Participants with HO reported significantly worse physical function, depression, pain interference and social integration scores than those without HO. After adjusting for covariables, participants with HO continued to report statistically significantly worse physical function than those without HO. Although physical functioning was consistently lower, the two populations did not differ significantly among psychosocial outcome measures.
CONCLUSIONS: While HO can result in physical limitations, the translation to psychosocial impairments was not evident. Targeted treatment of HO with the goal of maximizing physical function should be a focus of their rehabilitation.
LEVEL OF EVIDENCE: 2b TYPE OF STUDY: Symptom Prevalence Study.
PMID:38267289 | PMC:PMC11055684 | DOI:10.1016/j.burns.2024.01.017
J Burn Care Res. 2024 May 6;45(3):539-540. doi: 10.1093/jbcr/irae010.
NO ABSTRACT
PMID:38263288 | DOI:10.1093/jbcr/irae010
Ann Surg. 2024 May 1;279(5):874-879. doi: 10.1097/SLA.0000000000006146. Epub 2023 Nov 2.
ABSTRACT
OBJECTIVE: The aim of this study was to address the limited understanding of neuropathic pain (NP) among burn survivors by comprehensively examining its prevalence and related factors on a national scale using the Burn Model System (BMS) National Database.
BACKGROUND: NP is a common but underexplored complaint among burn survivors, greatly affecting their quality of life and functionality well beyond the initial injury. Existing data on NP and its consequences in burn survivors are limited to select single-institution studies, lacking a comprehensive national perspective.
METHODS: The BMS National Database was queried to identify burn patients responding to NP-related questions at enrollment, 6 months, 12 months, 2 years, and 5 years postinjury. Descriptive statistics and regression analyses were used to explore associations between demographic/clinical characteristics and self-reported NP at different time points.
RESULTS: There were 915 patients included for analysis. At discharge, 66.5% of patients experienced NP in their burn scars. Those with NP had significantly higher Patient-Reported Outcomes Measurement Information System 29 (PROMIS-29) pain inference, itch, anxiety, depression, and sleep disturbance scores and were less able to partake in social roles. Multiple logistic regression revealed male sex, % total body surface area, and moderate-to-severe pain as predictors of NP at 6 months. At 12 months, % total body surface area and moderate-to-severe pain remained significant predictors, while ethnicity and employment status emerged as significant predictors at 24 months.
CONCLUSIONS: This study highlights the significant prevalence of NP in burn patients and its adverse impacts on their physical, psychological, and social well-being. The findings underscore the necessity of a comprehensive approach to NP treatment, addressing both physical symptoms and psychosocial factors.
PMID:37916448 | PMC:PMC10997473 | DOI:10.1097/SLA.0000000000006146
Phys Med Rehabil Clin N Am. 2023 Nov;34(4):867-881. doi: 10.1016/j.pmr.2023.05.006. Epub 2023 Jun 25.
ABSTRACT
Burn injury commonly causes long-term physical impairments and psychosocial limitations that impact survivorship. This article uses the World Health Organization (WHO) International Classification of Functioning, Disability and Health (ICF) framework to summarize burn rehabilitation outcomes related to body functions and structures and how they relate to activities and participation within the social context. This article will contribute to a better understanding of burn recovery, facilitate the identification of specific and meaningful issues common to burn survivorship that may be under-reported in prior investigations and guide future rehabilitation to advance long-term burn outcomes.
PMID:37806703 | PMC:PMC10560762 | DOI:10.1016/j.pmr.2023.05.006
Burns. 2024 Feb;50(1):59-65. doi: 10.1016/j.burns.2023.08.014. Epub 2023 Aug 24.
ABSTRACT
INTRODUCTION: The association between military service history and long-term outcomes after burn injury is unknown. This study uses data from the Burn Model System National Database to compare outcomes of individuals with and without self-reported military service history.
METHODS: Outcome measures were assessed at 12 months after injury including the Veterans Rand-12 Item Health Survey/Short Form-12, Satisfaction With Life Scale, Patient Reported Outcomes Measure Information System 29, 4-D Itch scale, Post Traumatic Stress Disorder Check List - Civilian Version, self-reported Post Traumatic Stress Disorder, and employment status. This study included 675 people with burns of whom 108 reported a history of military service.
RESULTS: The military service history group was more likely to be older, and male. Those with military service were most likely to be on Medicare insurance and those without military service history were most likely to be on Private Insurance/HMP/PPO. No significant differences were found between those with and without military service history in the outcome measures.
CONCLUSIONS: Further research should examine differences in outcomes between civilians and those with military service history, including elements of resilience and post traumatic growth.
PMID:37709564 | PMC:PMC10872572 | DOI:10.1016/j.burns.2023.08.014
J Burn Care Res. 2024 Jan 5;45(1):136-144. doi: 10.1093/jbcr/irad136.
ABSTRACT
Physical, social, and psychological outcomes have been identified as relevant to the rehabilitation process of children with burn injuries. Existing legacy measures are limited in item content and only cover a few constructs. Condition-specific outcomes are highly relevant to gauge early growth and development. Computerized adaptive tests (CATs) leveraging advanced psychometric technologies minimize respondent burden. This project developed PS-LIBRE1-5 Profile CAT (Preschool Life Impact Burn Recovery Evaluation) to measure relevant postburn outcomes in children aged one to five. Responses to the field-tested PS-LIBRE1-5 Profile (188 items) were measured on a scale of frequency or ability. Scores were coded from 0 to 4 where higher scores reflected better functioning. Factor analysis identified the items retained in the final item bank of each scale. CAT simulations were conducted to estimate the mean score of each scale. The simulated CAT score and full item bank scores were compared based upon the score range, ceiling and floor effects, and marginal reliabilities. The child mean age was 3.0 ± 1.5 years (n = 500). Average burn size and time since burn injury were 4.2% TBSA and 1.1 years, respectively. Psychometric analysis resulted in eight scales: Physical, Communication and Language, Emotional Wellbeing, Mood, Anxiety, Peer Acceptance, Play, and Peer Relations. Ceiling effects were acceptable at <13% for all scales. Marginal reliabilities of the CATs were credible. The PS-LIBRE1-5 Profile CAT contains 111 items, and is a comprehensive measure that captures physical, communication and language, psychological, and social functioning of preschool burn survivors.
PMID:37703100 | PMC:PMC10872560 | DOI:10.1093/jbcr/irad136
J Surg Res. 2023 Nov;291:221-230. doi: 10.1016/j.jss.2023.06.005. Epub 2023 Jul 14.
ABSTRACT
INTRODUCTION: Upper airway management is crucial to burn care. Endotracheal intubation is often performed in the setting of inhalation injury, burns of the face and neck, or large burns requiring significant resuscitation. Tracheostomy may be necessary in patients requiring prolonged ventilatory support. This study compares long-term, patient-reported outcomes in burn patients with and without tracheostomy.
MATERIALS AND METHODS: Data from the Burn Model System Database, collected from 2013 to 2020, were analyzed. Demographic and clinical data were compared between those with and without tracheostomy. The following patient-reported outcomes, collected at 6-, 12-, and 24-mo follow-up, were analyzed: Veterans RAND 12-Item Health Survey (VR-12), Satisfaction with Life, Community Integration Questionnaire, Patient-Reported Outcomes Measurement Information System 29-Item Profile Measure, employment status, and days to return to work. Regression models and propensity-matched analyses were used to assess the associations between tracheostomy and each outcome.
RESULTS: Of 714 patients included in this study, 5.5% received a tracheostomy. Mixed model regression analyses demonstrated that only VR-12 Physical Component Summary scores at 24-mo follow-up were significantly worse among those requiring tracheostomy. Tracheostomy was not associated with VR-12 Mental Component Summary, Satisfaction with Life, Community Integration Questionnaire, or Patient-Reported Outcomes Measurement Information System 29-Item Profile Measure scores. Likewise, tracheostomy was not found to be independently associated with employment status or days to return to work.
CONCLUSIONS: This preliminary exploration suggests that physical and psychosocial recovery, as well as the ability to regain employment, are no worse in burn patients requiring tracheostomy. Future investigations of larger scale are still needed to assess center- and provider-level influences, as well as the influences of various hallmarks of injury severity. Nonetheless, this work should better inform goals of care discussions with patients and families regarding the use of tracheostomy in burn injury.
PMID:37454428 | PMC:PMC10528102 | DOI:10.1016/j.jss.2023.06.005
Arch Phys Med Rehabil. 2024 Feb;105(2):235-242. doi: 10.1016/j.apmr.2023.06.011. Epub 2023 Jun 30.
ABSTRACT
OBJECTIVE: To identify clinical factors (physical and psychological symptoms and post-traumatic growth) that predict social participation outcome at 24-month after burn injury.
DESIGN: A prospective cohort study based on Burn Model System National Database.
SETTING: Burn Model System centers.
PARTICIPANTS: 181 adult participants less than 2 years after burn injury (N=181).
INTERVENTIONS: Not applicable.
MAIN OUTCOME MEASURES: Demographic and injury variables were collected at discharge. Predictor variables were assessed at 6 and 12 months: Post-Traumatic Growth Inventory Short Form (PTGI-SF), Post-Traumatic Stress Disorder Checklist Civilian Version (PCL-C), Patient-Reported Outcomes Measurement Information System (PROMIS-29) Depression, Anxiety, Sleep Disturbance, Fatigue, and Pain Interference short forms, and self-reported Heat Intolerance. Social participation was measured at 24 months using the Life Impact Burn Recovery Evaluation (LIBRE) Social Interactions and Social Activities short forms.
RESULTS: Linear and multivariable regression models were used to examine predictor variables for social participation outcomes, controlling for demographic and injury variables. For LIBRE Social Interactions, significant predictors included the PCL-C total score at 6 months (β=-0.27, P<.001) and 12 months (β=-0.39, P<.001), and PROMIS-29 Pain Interference at 6 months (β=-0.20, P<.01). For LIBRE Social Activities, significant predictors consisted of the PROMIS-29 Depression at 6 months (β=-0.37, P<.001) and 12 months (β=-0.37, P<.001), PROMIS-29 Pain Interference at 6 months (β=-0.40, P<.001) and 12 months (β=-0.37, P<.001), and Heat Intolerance at 12 months (β=-4.55, P<.01).
CONCLUSIONS: Post-traumatic stress and pain predicted social interactions outcomes, while depression, pain and heat intolerance predicted social activities outcomes in people with burn injury.
PMID:37392780 | PMC:PMC10756920 | DOI:10.1016/j.apmr.2023.06.011
Rehabil Psychol. 2023 Aug;68(3):313-323. doi: 10.1037/rep0000508. Epub 2023 Jun 22.
ABSTRACT
INTRODUCTION: Understanding trajectories of recovery in key domains can be used to guide patients, families, and caregivers. The purpose of this study was to describe common trajectories of physical health over time and to examine predictors of these trajectories.
METHOD: Adults with burn injuries completed self-reported assessments of their health-related quality of life (HRQOL) as measured by the SF-12® Physical Component Summary (PCS) score at distinct time points (preinjury via recall, index hospital discharge, and at 6-, 12-, and 24 months after injury). Growth mixture modeling (GMM) was used to model PCS scores over time. Covariables included burn size, participant characteristics, and scores from the Community Integration Questionnaire (CIQ)/Social Integration portion, Satisfaction With Life Scale (SWLS), and Satisfaction With Appearance Scale (SWAP).
RESULTS: Data from 939 participants were used for complete-case analysis. Participants were 72% male, 64% non-Hispanic White, with an average age of 44 years and an average burn size of 20% of total body surface area (TBSA). The best fitting model suggested three distinct trajectories (Class 1 through 3) for HRQOL. We titled each Class according to the characteristics of their trajectory. Class 1 (recovering; n = 632), Class 2 (static; n = 77), and Class 3 (weakened; n = 205) reported near average HRQOL preinjury, then reported lower scores at discharge, with Class 1 subsequently improving to preinjury levels and Class 3 improving but not reaching their preinjury quality of life. Class 3 experienced the largest decrease in HRQOL. Class 2 reported the lowest preinjury HRQOL and remained low for the next 2 years, showing minimal change in their HRQOL.
CONCLUSIONS: These findings emphasize the importance of early universal screening and sustained intervention for those most at risk for low HRQOL following injury. For Class 2 (static), lower than average HRQOL before their injury is a warning. For Class 3 (weakened), if the scores at 6 months show a large decline, then the person is at risk for not regaining their HRQOL by 24 months and thus needs all available interventions to optimize their outcomes. Results of this study provide guidance for how to identify people with burn injury who would benefit from more intensive rehabilitation to help them achieve or regain better HRQOL. (PsycInfo Database Record (c) 2023 APA, all rights reserved).
PMID:37347905 | PMC:PMC10527858 | DOI:10.1037/rep0000508
J Burn Care Res. 2023 Nov 2;44(6):1419-1427. doi: 10.1093/jbcr/irad061.
ABSTRACT
This study examined the reliability and validity of the Patient Reported Outcomes Measurement System (PROMIS)-25, a profile instrument consisting of four-item fixed short forms for six health domains, in children living with burn injury. Data were provided by children participating in a multi-center longitudinal study of outcomes after burn injury. Floor and ceiling effects, unidimensionality, internal consistency, reliability, and differential item functioning (DIF) of the PROMIS-25 Profile v.2.0 were examined. Correlations with other established measures were calculated to assess concurrent validity. Children (n = 256) between the ages of 8-18 years with moderate to severe injury provided responses on PROMIS-25 domains. All PROMIS-25 domains showed high internal consistency. Substantial portions of the sample reported no symptoms (anxiety [58.2%], depressive symptoms [54.6%], fatigue [50.8%], pain [60.1%]). There was a large ceiling effect on peer relationships (46.8%) and physical function mobility (57.5%). One-factor confirmatory factor analyses supported unidimensionality for all domains. Reliability was sufficient for group mean comparisons (>0.8) across at least some trait levels for most domains except fatigue and anxiety. No DIF with respect to burn status was detected when comparing the burn sample to the PROMIS pediatric general U.S. population testing sample. These results provide evidence of reliability and validity of PROMIS-25 scores among children living with burn injury. Reliability of domains was low to moderate and would likely be improved, and ceiling effects reduced for some domains, by administering the PROMIS-37, which includes six items per domain.
PMID:37101360 | PMC:PMC10600322 | DOI:10.1093/jbcr/irad061
J Med Syst. 2023 Feb 16;47(1):26. doi: 10.1007/s10916-023-01914-7.
ABSTRACT
This review aims to identify and evaluate digital interventions for social participation in the growing population of adults with long-term physical conditions. Articles were sourced from MEDLINE, EMBASE, CINAHL and PsycINFO databases using subject headings and keywords related to "social participation" and "digital technology". Studies that adopted digital technology interventions to improve social participation in adults with long-term physical conditions were included. Data on study methodology, participant and digital intervention characteristics, and findings related to social participation were extracted. The search yielded a total of 4646 articles and 14 articles met criteria for final review with five randomized controlled trials, two non-randomized clinical trials and seven one-group pretest-posttest clinical trials. Studies were organized based on the digital intervention strategy implemented to improve social participation: group support (n = 4), individual skill training or counseling (n = 6), education and support (n = 3), and mixed intervention (n = 1). The group support interventions developed a social network among participants through videoconference, app, or virtual reality platform. Three studies reported positive improvements in different aspects of social participation. Individual skill training or counseling mainly utilized phone calls to help participants cope with activity participation and interpersonal relationship issues. Only two studies demonstrated benefits for social participation. The education and support intervention, which used messages and website information to increase participants' knowledge and provide support, showed positive findings in three studies. This review suggests digital interventions for improving social participation in adults with long-term physical conditions are feasible and the effectiveness of different strategies may vary.Registration: This review was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO) (registry number: CRD42021254105).
PMID:36792791 | PMC:PMC9931567 | DOI:10.1007/s10916-023-01914-7
J Head Trauma Rehabil. 2023 May-Jun 01;38(3):E186-E194. doi: 10.1097/HTR.0000000000000814. Epub 2022 Oct 14.
ABSTRACT
OBJECTIVE: The goal of this study is to describe national trends in inpatient rehabilitation facility (IRF) discharges for the most severely disabled cohort of patients with traumatic brain injury (TBI).
METHODS: Data from the Uniform Data System for Medical Rehabilitation for patients discharged from an IRF between January 1, 2002, and December 31, 2017, with a diagnosis of TBI and an admission Functional Independence Measure of 18, the lowest possible score, were obtained and analyzed.
RESULTS: Of the 252 112 patients with TBI discharged during the study period, 10 098 met the study criteria. From 2002 to 2017, the number of patients with an IRF admission Functional Independence Measure of 18 following TBI discharged from IRFs annually decreased from 649 to 488, modeled by a negative regression (coefficient = -2.97; P = .001), and the mean age (SD) increased from 43.0 (21.0) to 53.7 (21.3) years (coefficient = 0.70; P < .001). During the study period, the number of patients with the most severe disability on admission to IRF who were discharged annually as a proportion of total patients with TBI decreased from 5.5% to 2.5% (odds ratio = 0.95; P < .001) and their mean length of stay decreased from 41.5 (36.2) to 29.3 (24.9) days (coefficient = -0.83; P < .001].
CONCLUSION: The number and proportion of patients with the most severe disability on IRF admission following TBI who are discharged from IRFs is decreasing over time. This may represent a combination of primary prevention, early mortality due to withdrawal of life-sustaining treatment, alternative discharge dispositions, or changes in admitting and reimbursement practices. Furthermore, there has been a decrease in the duration of IRF level care for these individuals, which could ultimately lead to poorer functional outcomes, particularly given the importance of specialized rehabilitative care in this population.
PMID:36730991 | PMC:PMC10102246 | DOI:10.1097/HTR.0000000000000814
Shock. 2023 Mar 1;59(3):393-399. doi: 10.1097/SHK.0000000000002075. Epub 2023 Jan 4.
ABSTRACT
Introduction: Despite significant advances in pediatric burn care, bloodstream infections (BSIs) remain a compelling challenge during recovery. A personalized medicine approach for accurate prediction of BSIs before they occur would contribute to prevention efforts and improve patient outcomes. Methods: We analyzed the blood transcriptome of severely burned (total burn surface area [TBSA] ≥20%) patients in the multicenter Inflammation and Host Response to Injury ("Glue Grant") cohort. Our study included 82 pediatric (aged <16 years) patients, with blood samples at least 3 days before the observed BSI episode. We applied the least absolute shrinkage and selection operator (LASSO) machine-learning algorithm to select a panel of biomarkers predictive of BSI outcome. Results: We developed a panel of 10 probe sets corresponding to six annotated genes ( ARG2 [ arginase 2 ], CPT1A [ carnitine palmitoyltransferase 1A ], FYB [ FYN binding protein ], ITCH [ itchy E3 ubiquitin protein ligase ], MACF1 [ microtubule actin crosslinking factor 1 ], and SSH2 [ slingshot protein phosphatase 2 ]), two uncharacterized ( LOC101928635 , LOC101929599 ), and two unannotated regions. Our multibiomarker panel model yielded highly accurate prediction (area under the receiver operating characteristic curve, 0.938; 95% confidence interval [CI], 0.881-0.981) compared with models with TBSA (0.708; 95% CI, 0.588-0.824) or TBSA and inhalation injury status (0.792; 95% CI, 0.676-0.892). A model combining the multibiomarker panel with TBSA and inhalation injury status further improved prediction (0.978; 95% CI, 0.941-1.000). Conclusions: The multibiomarker panel model yielded a highly accurate prediction of BSIs before their onset. Knowing patients' risk profile early will guide clinicians to take rapid preventive measures for limiting infections, promote antibiotic stewardship that may aid in alleviating the current antibiotic resistance crisis, shorten hospital length of stay and burden on health care resources, reduce health care costs, and significantly improve patients' outcomes. In addition, the biomarkers' identity and molecular functions may contribute to developing novel preventive interventions.
PMID:36597771 | PMC:PMC9991965 | DOI:10.1097/SHK.0000000000002075
J Burn Care Res. 2023 Jan 5;44(1):222-223. doi: 10.1093/jbcr/irac172.
NO ABSTRACT
PMID:36371723 | PMC:PMC9839542 | DOI:10.1093/jbcr/irac172
J Am Med Dir Assoc. 2022 Dec;23(12):1964-1970. doi: 10.1016/j.jamda.2022.08.005. Epub 2022 Sep 21.
ABSTRACT
OBJECTIVES: Readmission to acute care from the inpatient rehabilitation facility (IRF) setting is potentially preventable and an important target of quality improvement and cost savings. The objective of this study was to develop a risk calculator to predict 30-day all-cause readmissions from the IRF setting.
DESIGN: Retrospective database analysis using the Uniform Data System for Medical Rehabilitation (UDSMR) from 2015 through 2019.
SETTING AND PARTICIPANTS: In total, 956 US inpatient rehabilitation facilities and 1,849,768 IRF discharges comprising patients from 14 impairment groups.
METHODS: Logistic regression models were developed to calculate risk-standardized 30-day all-cause hospital readmission rates for patients admitted to an IRF. Models for each impairment group were assessed using 12 common clinical and demographic variables and all but 4 models included various special variables. Models were assessed for discrimination (c-statistics), calibration (calibration plots), and internal validation (bootstrapping). A readmission risk scoring system was created for each impairment group population and was graphically validated.
RESULTS: The mean age of the cohort was 68.7 (15.2) years, 50.7% were women, and 78.3% were Caucasian. Medicare was the primary payer for 73.1% of the study population. The final models for each impairment group included between 4 and 13 total predictor variables. Model c-statistics ranged from 0.65 to 0.70. There was good calibration represented for most models up to a readmission risk of 30%. Internal validation of the models using bootstrap samples revealed little bias. Point systems for determining risk of 30-day readmission were developed for each impairment group.
CONCLUSIONS AND IMPLICATIONS: Multivariable risk factor algorithms based upon administrative data were developed to assess 30-day readmission risk for patients admitted from IRF. This report represents the development of a readmission risk calculator for the IRF setting, which could be instrumental in identifying high risk populations for readmission and targeting resources towards a diverse group of IRF impairment groups.
PMID:36150407 | PMC:PMC9926973 | DOI:10.1016/j.jamda.2022.08.005
N Engl J Med. 2022 Aug 18;387(7):581-583. doi: 10.1056/NEJMp2205162. Epub 2022 Aug 13.
NO ABSTRACT
PMID:35960203 | PMC:PMC10064866 | DOI:10.1056/NEJMp2205162
J Burn Care Res. 2023 May 2;44(3):624-630. doi: 10.1093/jbcr/irac112.
ABSTRACT
Geospatial proximity to American Burn Association (ABA)-verified burn centers or self-designated burn care facilities varies across the country. This study evaluates the effect of distance to treatment center on long-term, patient-reported outcomes. Data from the Burn Model System (BMS) National Longitudinal Database were analyzed. Demographic and clinical data were compared between three cohorts stratified by distance to BMS center (<20, 20-49.9, ≥50 miles). Distance to BMS center was calculated as driving distance between discharge and BMS center ZIP code centroids. The following patient-reported outcomes, collected at 12-months follow-up, were examined: Veterans RAND 12-Item Health Survey (VR-12), Satisfaction with Life (SWL) scale, employment status, and days to return to work. Mixed model regression analyses were used to examine the associations between distance to BMS center and each outcome, controlling for demographic and clinical variables. Of 726 patients included in this study, 26.3% and 28.1% were <20 and between 20 and 49.9 miles to a BMS center, respectively; 46.6% were ≥50 miles to a BMS center. Greater distance was associated with white/non-Hispanic race/ethnicity, preinjury employment, flame injury, and larger burn size (P < .001). Regression analyses did not identify significant associations between distance to BMS center and any patient-reported outcomes. This study suggests that patients treated at BMS centers have similar long-term, patient-reported outcomes of physical and psychosocial function, as well as employment, despite centralization of burn care and rehabilitation services. Given a steady decline in the incidence of burn injury, continued concentration of key resources is logical and safe.
PMID:35939346 | PMC:PMC9905382 | DOI:10.1093/jbcr/irac112
J Burn Care Res. 2023 Jan 5;44(1):27-34. doi: 10.1093/jbcr/irac088.
ABSTRACT
Individuals who experience burns are at higher risk of developing posttraumatic stress disorder and chronic pain. A synergistic relationship exists between posttraumatic stress disorder and chronic pain. We sought to evaluate the role of individual posttraumatic stress disorder symptom clusters as predictors of pain interference. We hypothesized that the hyperarousal and emotional numbing symptom clusters would be predictive of pain interference, even when accounting for the other two posttraumatic stress disorder symptom clusters, pain intensity, and other covariates. Multivariate linear regression analyses were completed using data from the Burn Model System National Database. A total of 439 adult participants had complete responses on self-report measures assessing posttraumatic stress disorder symptoms, pain intensity, and pain interference at 6-month after discharge and were included in analyses. Results indicate hyperarousal (B = .10, p = .03) and emotional numbing (B = .13, p = .01) posttraumatic stress disorder symptom clusters were each significantly associated with pain interference, even when accounting for pain intensity (B = .64, p < .001). Results highlight the importance of the emotional numbing and hyperarousal posttraumatic stress disorder symptom clusters in explaining pain interference. Findings suggest that when posttraumatic stress disorder symptoms or chronic pain are present, screening for and treating either condition may be warranted to reduce pain interference. Further, psychological interventions that target emotional numbing and hyperarousal posttraumatic stress disorder symptoms may be fruitful for promoting better coping with chronic pain and reducing pain interference.
PMID:35866527 | PMC:PMC9990905 | DOI:10.1093/jbcr/irac088
Burns. 2023 May;49(3):688-700. doi: 10.1016/j.burns.2022.05.010. Epub 2022 May 16.
ABSTRACT
INTRODUCTION: Health Related Quality of Life (HRQoL) surveys such as PROMIS-29 may facilitate shared decision-making regarding surgery after burn injury. We aimed to examine whether scar revision and contracture release surgery after index hospitalization was associated with differences in HRQoL.
METHODS: Patient and PROMIS-29 Profile v2.0 data were extracted from the Burn Model System (BMS) at 6-, 12-, and 24-months after burn. PROMIS-29 measures 7 health-related domains. Linear regression was performed to identify associations between independent burn patient variables (e.g. scar-related surgery) and PROMIS-29 scores. Socio-demographic and injury variables were analyzed using logistic regression to determine the likelihood of undergoing burn-related surgery.
RESULTS: Of 727 participants, 201 (27.6%) underwent ≥ 1 scar/contracture operation within 24 months of injury. Number of operations at index hospital admission and range of motion (ROM) deficit at discharge were correlated with an increased likelihood of undergoing subsequent scar/contracture surgery (p < 0.05). Participants undergoing scar/contracture surgery and those that were Medicaid insured reported significantly worse HRQoL for PROMIS domains: anxiety, depression, and fatigue (p < 0.05).
CONCLUSIONS: After adjusting for burn severity and available confounders, participants who underwent scar-related burn reconstructive surgery after index hospitalization reported overall worse Health-Related Quality of Life (HRQoL) in multiple domains.
PMID:35718573 | DOI:10.1016/j.burns.2022.05.010
J Burn Care Res. 2023 Mar 2;44(2):363-372. doi: 10.1093/jbcr/irac079.
ABSTRACT
Disparities in socioeconomic status and minority status affect the risk of burn injury and the severity of that injury, thus affecting the subsequent cost of care. We aimed to characterize the demographic details surrounding receipt of financial assistance due to burn injury and its relationship with health-related quality of life scores. Participants ≥18 from Burn Model System National Longitudinal Database (BMS) with complete demographic data were included (n = 4330). Nonresponders to financial assistance questions were analyzed separately. The remaining sample (n = 1255) was divided into participants who received financial assistance because of burn injury, those who received no financial assistance, and those who received financial assistance before injury and as a result of injury. A demographic and injury-characteristic comparison was conducted. Health-related quality of life metrics (Satisfaction with Life, Short Form-12/Veterans RAND 12-Item Health Survey, Community Integration Questionnaire Social Component, and the Post-Traumatic Growth Inventory) were analyzed preinjury, then 6-months, 1-year, and 2-years postinjury. A matched cohort analysis compared these scores. When compared to their no financial assistance counterparts, participants receiving financial assistance due to burns were more likely to be minorities (19% vs 14%), have more severe injuries (%TBSA burn 21% vs 10%), and receive workers' compensation (24% vs 9%). They also had lower health-related quality of life scores on all metrics except the post-traumatic growth inventory. Financial assistance may aid in combating disparities in posttraumatic growth scores for participants at the greatest risk of financial toxicity but does not improve other health-related quality of life metrics.
PMID:35699664 | DOI:10.1093/jbcr/irac079
Burns. 2022 Aug;48(5):1262-1266. doi: 10.1016/j.burns.2022.04.003. Epub 2022 Apr 22.
NO ABSTRACT
PMID:35504767 | PMC:PMC9357168 | DOI:10.1016/j.burns.2022.04.003
Burns. 2022 Jun;48(4):824-832. doi: 10.1016/j.burns.2022.03.001. Epub 2022 Mar 11.
ABSTRACT
OBJECTIVE: Increased body weight has been associated with reduced muscle wasting in the early catabolic phase after a severe burn. Yet, overweight and obese non-burn children often exhibit impaired musculoskeletal function, which may lead to poor physical function (PF). We aimed to determine the association between body mass index (BMI) at discharge and self-reported PF and caregiver proxy-reported PF during recovery of burned children.
MATERIALS AND METHODS: This is a retrospective multisite longitudinal study in paediatric burn patients ((8-17 y old at time of burn). PF outcome measures were self-reported mobility, proxy-reported mobility, and upper extremity PF evaluated using PROMIS measures at 6-, 12-, and 24-months after injury. Primary exposure variable was BMI-for-age at discharge.
RESULTS: A total of 118 paediatric patients, aged 11.7 ± 3.3 y, with burns covering 37.6 ± 18.8% of their total body surface area (TBSA) and BMI-for-age of 23.1 ± 5.4 kg/m2 at discharge were analyzed. BMI at discharge was not significantly associated with self-reported mobility scores 6 months after burn (beta coefficient =-0.23, p = 0.31), had a positive effect on mobility at 12 months (beta = 0.46, p = 0.05), and no effect at 24 months after injury (beta=-0.10, p = 0.60), when adjusted for burn size. BMI did not have a significant effect on proxy-reported mobility or upper extremity PF.
CONCLUSION: A greater BMI at discharge was associated with improved self-reported PF at 12 months after burn but not at 6 months or 24 months, which suggests a faster recovery of PF in paediatric patients of larger body weight. Our data suggests that a larger body weight does not compromise the recovery of PF after burn.
PMID:35410694 | PMC:PMC9232948 | DOI:10.1016/j.burns.2022.03.001
Front Pain Res (Lausanne). 2021 Jul 12;2:697475. doi: 10.3389/fpain.2021.697475. eCollection 2021.
ABSTRACT
Introduction: Adequate pain management for inpatients in rehabilitation units is essential for achieving therapeutic goals. Opioid treatments are commonly prescribed, but these are associated with numerous adverse effects, including the risk of addiction and decreased quality of life. Conditioning an open-label placebo is a promising approach to extend the analgesic effect of the opioid while reducing its overall dosage. Objectives: To describe a patient's experience in using conditioning open-label placebo (COLP) as a pharmaco-behavioral intervention to decrease opioid intake and its side effects after inpatient rehabilitation discharge, and to perform a literature review about the use of open-label placebo in pain. Methods: This case study has been extracted from a clinical trial initiated in 2018. A 61-year-old male was recruited at a tertiary rehabilitation hospital after suffering a traumatic sport-related injury and orthopedic surgery. Pain management included prescription of non-steroidal anti-inflammatory drugs (NSAIDs) and short-acting oxycodone. After trial participation, the patient requested off-label COLP treatment to help him decrease outpatient opioid utilization. Results: After COLP treatment, the patient could discontinue oxycodone intake (a reduction from 15 morphine equivalents/day) after rehabilitation discharge. Moreover, opioid side effects decreased from 46 to 9 points on the numerical opioid side-effects scale. A literature review identified five clinical trials using "honest" open-label placebo (OLP) or COLP as an experimental intervention for pain control. From these studies, two were in the area of chronic lower back pain, one in post spine surgery, one in irritable bowel syndrome, and another in spinal cord injury and polytrauma. Four studies reported positive outcomes related to pain control, while one study showed no significant differences in pain management between treatment-as-usual and the COLP group. Conclusion: The case report illustrates how a pharmaco-behavioral intervention can facilitate downward opioid titration safely after inpatient rehabilitation. It initiates a discussion about new approaches for opioid management using conditioning and the patient's expectation of pain relief.
PMID:35295534 | PMC:PMC8915754 | DOI:10.3389/fpain.2021.697475
Arch Phys Med Rehabil. 2022 May;103(5):1051-1052. doi: 10.1016/j.apmr.2022.01.138. Epub 2022 Jan 31.
NO ABSTRACT
PMID:35093330 | DOI:10.1016/j.apmr.2022.01.138
J Trauma Acute Care Surg. 2022 Jun 1;92(6):1066-1074. doi: 10.1097/TA.0000000000003547. Epub 2022 Jan 25.
ABSTRACT
BACKGROUND: People living with burn injury often face long-term physical and psychological sequelae associated with their injuries. Few studies have examined the impacts of burn injuries on long-term health and function, life satisfaction, and community integration beyond 5 years postinjury. The purpose of this study was to examine these outcomes up to 20 years after burn injury.
METHODS: Data from the Burn Model System National Longitudinal Database (1993-2020) were analyzed. Patient-reported outcome measures were collected at discharge (preinjury status recall) and 5 years, 10 years, 15 years, and 20 years after injury. Outcomes examined were the SF-12/VR-12 Physical Component Summary and Mental Component Summary, Satisfaction with Life Scale, and Community Integration Questionnaire. Trajectories were developed using linear mixed models with repeated measures of outcome scores over time, controlling for demographic and clinical variables.
RESULTS: The study population included 421 adult burn survivors with a mean age of 42.4 years. Lower Physical Component Summary scores (worse health) were associated with longer length of hospital stay, older age at injury and greater time since injury. Similarly, lower Mental Component Summary scores were associated with longer length of hospital stay, female sex, and greater time since injury. Satisfaction with Life Scale scores decrease negatively over time. Lower Community Integration Questionnaire scores were associated with burn size and Hispanic/Latino ethnicity.
CONCLUSION: Burn survivors' physical and mental health and satisfaction with life worsened over time up to 20 years after injury. Results strongly suggest that future studies should focus on long-term follow-up where clinical interventions may be necessary.
LEVEL OF EVIDENCE: Prognostic and Epidemiologic; Level III.
PMID:35081598 | PMC:PMC9133040 | DOI:10.1097/TA.0000000000003547
J Burn Care Res. 2022 Sep 1;43(5):1095-1104. doi: 10.1093/jbcr/irab245.
ABSTRACT
Trajectory curves are valuable tools to benchmark patient health status and predict future outcomes. A longitudinal study is underway to examine social participation after burn injury using the Life Impact Burn Recovery Evaluation (LIBRE) Profile with the goal of developing trajectory curves for specific domains that focus on social reintegration. We conducted a scoping review to inform and understand trajectory curves applied in clinical settings to compare outcomes for an individual to a matched cohort of comparable patients or predicted expected outcomes over time. This scoping review utilized a PubMed search from January 2014 to August 2019 for the following terms: "trajectory curves" or "trajectory models" and "clinic" or "clinical." Only articles that specifically referenced longitudinal and clinical research designs were included in the scoping review. Articles were assessed using standard scoping review methods and categorized based on clinical application of trajectory curves for either benchmarking or prediction. The initial literature review identified 141 manuscripts and 34 met initial inclusion criteria. The reviewed articles support the clinical use of trajectory curves. Findings provide insight into several key determinants involved with the successful development and implementation of trajectory curves in clinical settings. These findings will inform efforts to use the LIBRE Profile to model social participation recovery and assist in developing effective strategies using trajectory curves to promote social reintegration after burn injury.
PMID:34986488 | PMC:PMC9255662 | DOI:10.1093/jbcr/irab245
J Burn Care Res. 2022 Sep 1;43(5):1114-1128. doi: 10.1093/jbcr/irab247.
ABSTRACT
The transition from early childhood to teen years (5-12) is a critical time of development, which can be made particularly challenging by a burn injury. Assessing postburn recovery during these years is important for improving pediatric survivors' development and health outcomes. Few validated burn-specific measures exist for this age group. The purpose of this study was to generate item pools that will be used to create a future computerized adaptive test (CAT) assessing postburn recovery in school-aged children. Item pool development was guided by the previously developed School-Aged Life Impact Burn Recovery Evaluation (SA-LIBRE5-12) conceptual framework. The item pool development process involved a systematic literature review, extraction of candidate items from existing legacy measures, iterative item review during expert consensus meetings, and parent cognitive interviews. The iterative item review with experts consisted of six rounds. A total of 10 parent cognitive interviews were conducted. The three broad themes of concern were items that needed 1) clarification, needed context, or were vague, 2) age dependence and relevance, and 3) word choice. The cognitive interviews indicated that survey instructions, recall period, item stem, and response choices were interpretable by respondents. Final item pool based on parental feedback consists of 57, 81, and 60 items in physical, psychological, and family and social functioning, respectively. Developed item pools (n = 198) in three domains are consistent with the existing conceptual framework. The next step involves field testing the item pool and calibration using item response theory to develop and validate the SA-LIBRE5-12 CAT Profile.
PMID:34965302 | PMC:PMC9255664 | DOI:10.1093/jbcr/irab247
Burns. 2022 Mar;48(2):460-462. doi: 10.1016/j.burns.2021.11.025. Epub 2021 Dec 2.
NO ABSTRACT
PMID:34924225 | PMC:PMC9275732 | DOI:10.1016/j.burns.2021.11.025
J Burn Care Res. 2022 Mar 23;43(2):343-352. doi: 10.1093/jbcr/irab225.
ABSTRACT
Acute pediatric burn injuries often result in chronic sequelae that affect physical, psychological, and social outcomes. To date, no review has comprehensively reported on the impact of burn injuries across all three domains in school-aged children. The aim of this systematic review was to identify published literature that focuses on the impact of burn injuries on physical, psychological, or social functioning, and report upon the nature of study characteristics and their outcomes. We included literature published after 1980, focusing on burn outcomes in children aged 5 to 18 years. Each eligible study was systematically reviewed and primary outcomes were classified into outcome domains based on existing frameworks. Fifty-eight studies met inclusion criteria, and reported on physical (n = 24), psychological (n = 47), and social (n = 29) domains. The majority of the studies had sample sizes of <100 participants, burn size of <40%, and findings reported by parents and/or burn survivors. Only eight of 107 different measures were used in three or more studies. Parents and burn survivors generally reported better physical and social outcomes and worse psychological functioning compared to non-burn populations. Physical disabilities were associated with psychological and social functioning in several studies. Follow-up data reported improvements across domains. This review demonstrates the importance of physical, psychological, and social status as long-term outcomes in burn survivors. Mixed findings across three outcome domains warrant long-term research. Findings of this review will guide the foundation of comprehensive burn and age-specific instruments to assess burn recovery.
PMID:34922361 | PMC:PMC9272085 | DOI:10.1093/jbcr/irab225
Burns. 2022 Mar;48(2):485-486. doi: 10.1016/j.burns.2021.11.008. Epub 2021 Nov 16.
ABSTRACT
AThe exceptionally severe burns caused by incendiary weapons make strengthening international law a humanitarian imperative. Given healthcare professionals' deep understanding of the human cost of burn injuries, they are in a unique position to urge governments to initiate a process to assess the law's shortcomings at a major UN disarmament meeting in December. One way to advocate for such policy change is by signing an open letter from healthcare professionals and burn survivor organizations.
PMID:34903413 | DOI:10.1016/j.burns.2021.11.008
Arch Phys Med Rehabil. 2022 May;103(5):851-857. doi: 10.1016/j.apmr.2021.11.003. Epub 2021 Nov 29.
ABSTRACT
OBJECTIVE: To describe differences in characteristics and outcomes of patients with traumatic brain injury by inpatient rehabilitation facility (IRF) profit status.
DESIGN: Retrospective database review using the Uniform Data System for Medical Rehabilitation.
SETTING: IRFs.
PARTICIPANTS: Individual discharges (N=53,630) from 877 distinct rehabilitation facilities for calendar years 2016 through 2018.
INTERVENTION: Not applicable.
MAIN OUTCOME MEASURES: Patient demographic data (age, race, primary payer source), admission and discharge FIM, FIM gain, length of stay efficiency, acute hospital readmission from for-profit and not-for-profit IRFs within 30 days, and community discharges by facility profit status.
RESULTS: Patients at for-profit facilities were significantly older (69.69 vs 64.12 years), with lower admission FIM scores (52 vs 57), shorter lengths of stay (13 vs 15 days), and higher discharge FIM scores (88 vs 86); for-profit facilities had higher rates of community discharges (76.8% vs 74.6%) but also had higher rates of readmission (10.3% vs 9.9%).
CONCLUSIONS: The finding that for-profit facilities admit older patients who are reportedly less functional on admission and more functional on discharge, with higher rates of community discharge but higher readmission rates than not-for-profit facilities is an unexpected and potentially anomalous finding. In general, older, less functional patients who stay for shorter periods of time would not necessarily be expected to make greater functional gains. These differences should be further studied to determine if differences in patient selection, coding and/or billing, or other unreported factors underlie these differences.
PMID:34856156 | DOI:10.1016/j.apmr.2021.11.003
Arch Phys Med Rehabil. 2022 Mar;103(3):424-429. doi: 10.1016/j.apmr.2021.10.019. Epub 2021 Nov 9.
ABSTRACT
OBJECTIVE: To obtain useful information for clinicians in evaluating patients with brain tumors for transfer to and subsequent care in inpatient rehabilitation facilities (IRFs).
DESIGN: Retrospective chart review.
SETTING: Inpatient rehabilitation facility.
PARTICIPANTS: A total of 208 adults with either initial or recurrent brain tumors who were admitted to an IRF between January 2017 and December 2018 after an acute hospitalization.
INTERVENTIONS: None MAIN OUTCOME MEASURES: Transfer from an IRF to an acute care hospital and mortality within 6 months from admission to an IRF.
RESULTS: Of the 208 patients who met inclusion criteria, 20.2% were transferred to an acute care hospital during the IRF stay, which was associated with prior chemotherapy, steroid use, and laterality of tumor. In total, 36.9% of patients with brain tumors died within 6 months of an IRF admission that was associated with recurrent tumor diagnosis, prior chemotherapy, prior neurosurgical intervention, prior neurostimulant use, use of steroids, isocitrate dehydrogenase and O6-methyl-guanyl-methyl-transferase biomarkers, and laterality and location of tumor.
CONCLUSIONS: Patients with brain tumors have a notable potential for acute hospital transfer and mortality within 6 months of IRF stay, with several tumor- and treatment-related risk factors. This information can help identify functional goals, identify high risk patients, enable closer clinical monitoring, and facilitate focused care discussions at IRFs.
PMID:34762854 | PMC:PMC9446107 | DOI:10.1016/j.apmr.2021.10.019
J Burn Care Res. 2022 Jul 1;43(4):899-905. doi: 10.1093/jbcr/irab215.
ABSTRACT
Depression and posttraumatic stress (DPTS) are common psychiatric comorbidities following burn injury. The purpose of this study was to develop an admission scoring system that assesses the risk of development of depression or posttraumatic symptoms in the burn population. This study is a retrospective review of the prospectively collected Burn Model System National Database. Adult burn survivors enrolled from 2014 to 2018 (n = 486) were included. The primary outcome was the presence of DPTS symptoms at 6, 12, or 24 months postinjury. Logistic regression analysis was used to identify demographic and clinical predictors of DPTS symptoms. A risk scoring system was then created based on assigning point values to relevant predictor factors. The study population had a mean age of 46.5 ± 15.8 years, mean burn size of 18.3 ± 19.7%, and was 68.3% male. Prior to injury, 71.3% of the population was working, 47.9% were married, and 50.8% had completed more than a high school education. An 8-point risk scoring system was developed using the following predictors of DPTS symptom development: gender, psychiatric treatment in the past year, graft size, head/neck graft, etiology of injury, and education level. This study is the first to develop a DPTS symptom risk scoring system for burn injury. This scoring system will aid in identifying burn survivors at high risk of long-term psychiatric symptoms that may be used to improve screening, monitoring, timely diagnosis, and interventions.
PMID:34751379 | PMC:PMC9201555 | DOI:10.1093/jbcr/irab215
J Burn Care Res. 2022 May 17;43(3):602-612. doi: 10.1093/jbcr/irab190.
ABSTRACT
The Burn Specific Health Scale-Brief (BSHS-B) is a commonly used burn-specific health outcome measure that includes 40 items across nine subscales. The objective of this study was to use both classical and modern psychometric methods to evaluate psychometric properties of the BSHS-B. Data were collected postburn injury by a multisite federally funded project tracking long-term outcomes. We examined dimensionality, local dependence, item fit, and functioning of response categories, homogeneity, and floor and ceiling effects. Items were fit to Item Response Theory models for evaluation. A total of 653 adults with burn injury completed the BSHS-B. Factor analyses supported unidimensionality for all subscales, but not for a total score based on all 40 items. All nine of the subscales had significant ceiling effects. Six item pairs displayed local dependence suggesting redundance and 11 items did not fit the Item Response Theory models. At least 15 items have too many response options. Results identified numerous psychometric issues with the BSHS-B. A single summary score should never be used for any purpose. Psychometric properties of the scale need to be improved by removing redundant items, reducing response categories, and modifying or deleting problematic items. Additional conceptual work is needed to, at a minimum, revise the work subscale and optimally to revisit and clearly define the constructs measured by all the subscales. Additional items are needed to address ceiling effects.
PMID:34643699 | PMC:PMC9165660 | DOI:10.1093/jbcr/irab190
J Burn Care Res. 2022 Mar 23;43(2):293-299. doi: 10.1093/jbcr/irab170.
ABSTRACT
The costs required to provide acute care for patients with serious burn injuries are significant. In the United States, these costs are often shared by patients. However, the impacts of preinjury finances on health-related quality of life (HRQL) have been poorly characterized. We hypothesized that lower income and public payers would be associated with poorer HRQL. Burn survivors with complete data for preinjury personal income and payer status were extracted from the longitudinal Burn Model System National Database. HRQL outcomes were measured with VR-12 scores at 6, 12, and 24 months postinjury. VR-12 scores were evaluated using generalized linear models, adjusting for potential confounders (eg, age, sex, self-identified race, burn injury severity). About 453 participants had complete data for income and payer status. More than one third of BMS participants earned less than $25,000/year (36%), 24% earned $25,000 to 49,000/year, 23% earned $50,000 to 99,000/year, 11% earned $100,000 to 149,000/year, 3% earned $150,000 to 199,000/year, and 4% earned more than $200,000/year. VR-12 mental component summary (MCS) and physical component summary (PCS) scores were highest for those who earned $150,000 to 199,000/year (55.8 and 55.8) and lowest for those who earned less than $25,000/year (49.0 and 46.4). After adjusting for demographics, payer, and burn severity, 12-month MCS and PCS and 24-month PCS scores were negatively associated with Medicare payer (P < .05). Low income was not significantly associated with lower VR-12 scores. There was a peaking relationship between HRQL and middle-class income, but this trend was not significant after adjusting for covariates. Public payers, particularly Medicare, were independently associated with poorer HRQL. The findings might be used to identify those at risk of financial toxicity for targeting assistance during rehabilitation.
PMID:34519793 | PMC:PMC10026600 | DOI:10.1093/jbcr/irab170
J Burn Care Res. 2022 May 17;43(3):640-645. doi: 10.1093/jbcr/irab161.
ABSTRACT
Burn scar contracture (BSC) is a common pathological outcome following burn injuries, leading to limitations in range of motion (ROM) of affected joints and impairment in function. Despite a paucity of research addressing its efficacy, static splinting of affected joints is a common preventative practice. A survey of therapists performed 25 years ago showed a widely divergent practice of splinting during the acute burn injury. We undertook this study to determine the current practice of splinting during the index admission for burn injuries. This is a review of a subset of patients enrolled in the Burn Patient Acuity Demographics, Scar Contractures and Rehabilitation Treatment Related to Patient Outcome Study (ACT) database. ACT was an observational multicenter study conducted from 2010 to 2013. The most commonly splinted joints (elbow, wrist, knee, and ankle) and their seven motions were included. Variables included patients' demographics, burn variables, rehabilitation treatment, and hospital course details. Univariate and multivariate analysis of factors related to splinting was performed. P < .05 was significant. Thirty percent of the study population (75 patients) underwent splinting during their hospitalization. Splinting was associated with larger burns and increased injury severity on the patient level and increased involvement with burns requiring grafting in the associated cutaneous functional unit (CFU) on the joint level. The requirement for skin grafting in both analyses remained independently related to splinting, with requirement for grafting in the associated CFU increasing the odds of splinting six times (OR = 6.0, 95% CI = 3.8-9.3, P < .001). On average, splinting was initiated about a third into the hospital length of stay (LOS, 35 ± 21% of LOS) and splints were worn for 50% (50 ± 26%) of the LOS. Joints were splinted for an average 15.1 ± 4.8 hours a day. The wrist was most frequently splinted joint being splinted with one third of wrists splinted (30.7%) while the knee was the least frequently splinted joint with 8.2% splinted. However, when splinted, the knee was splinted the most hours per day (17.6 ± 4.8 hours) and the ankle the least (14.4 ± 4.6 hours). Almost one third had splinting continued to discharge (20, 27%). The current practice of splinting, especially the initiation, hours of wear and duration of splinting following acute burn injury remains variable. Splinting is independently related to grafting, grafting in the joint CFU, larger CFU involvement and is more likely to occur around the time of surgery. A future study looking at splinting application and its outcomes is warranted.
PMID:34490885 | DOI:10.1093/jbcr/irab161
J Burn Care Res. 2021 Nov 24;42(6):1081-1086. doi: 10.1093/jbcr/irab139.
ABSTRACT
Burn survivors experience barriers to returning to work. For those who do return to work, little is known regarding whether they achieve preinjury productivity (i.e., equivalent or gain in income compared to preinjury income). Identifying patients at risk of not achieving preinjury productivity is important for targeting services that support this population. They extracted occupational and income data through 24 months postinjury from the multicenter, longitudinal Burn Model System National Database. Annual income was reported in six groups: <$25k, $25k-50k, $50k-99k, $100k-149k, $150k-199k, and $>199k. Participants were classified by change in income at each follow-up (i.e., gain, loss, and equivalent). Explanatory variables included demographics, injury characteristics, insurance payer, employment status, and job type. Multilevel, multivariable logistic regression was used to model return to productivity. Four hundred fifty-three participants provided complete income data at discharge and follow-up. Of the 302 participants employed preinjury, 180 (60%) returned to work within 24 months postinjury. Less than half (138) returned to productivity (46% of participants employed preinjury; 77% of those who returned to work). Characteristics associated with return to productivity included older age (median 46.9 vs 45.9 years, OR 1.03, P = .006), Hispanic ethnicity (24% vs 11%, OR 1.80, P = 0.041), burn size >20% TBSA (33.7% vs 33.0%, OR 2.09, P = 0.045), and postinjury employment (54% vs 26%, OR 3.41, P < 0.001). More than half of employed people living with burn injury experienced loss in productivity within 24 months postinjury. Even if they return to work, people living with burn injuries face challenges returning to productivity and may benefit from vocational rehabilitation and/or financial assistance.
PMID:34302467 | PMC:PMC9255661 | DOI:10.1093/jbcr/irab139
J Trauma Acute Care Surg. 2022 Jan 1;92(1):213-222. doi: 10.1097/TA.0000000000003365.
ABSTRACT
BACKGROUND: Patient-reported outcomes are important for understanding recovery after burn injury, benchmarking service delivery and measuring the impact of interventions. Patient-Reported Outcomes Measurement Information System (PROMIS)-29 domains have been validated for use among diverse populations though not among burn survivors. The purpose of this study was to examine validity and reliability of PROMIS-29 scores in this population.
METHODS: The PROMIS-29 scores of physical function, anxiety, depression, fatigue, sleep disturbance, ability to participate in social roles, and pain interference were evaluated for validity and reliability in adult burn survivors. Unidimensionality, floor and ceiling effects, internal consistency, and reliability were examined. Differential item functioning was used to examine bias with respect to demographic and injury characteristics. Correlations with measures of related constructs (Community Integration Questionnaire, Satisfaction with Life Scale, Post-Traumatic Stress Checklist-Civilian, and Veteran's Rand-12) and known-group differences were examined.
RESULTS: Eight hundred and seventy-six burn survivors with moderate to severe injury from 6 months to 20 years postburn provided responses on PROMIS-29 domains. Participants' ages ranged from 18 years to 93 years at time of assessment; mean years since injury was 3.4. All PROMIS domain scores showed high internal consistency (Cronbach's α = 0.87-0.97). There was a large ceiling effect on ability to participate in social roles (39.7%) and physical function (43.3%). One-factor confirmatory factor analyses supported unidimensionality (all comparative fit indices >0.95). We found no statistically significant bias (differential item functioning). Reliability was high (>0.9) across trait levels for all domains except sleep, which reached moderate reliability (>0.85). All known-group differences by demographic and clinical characteristics were in the hypothesized direction and magnitude except burn size categories.
CONCLUSION: The results provide strong evidence for reliability and validity of PROMIS-29 domain scores among adult burn survivors. Reliability of the extreme scores could be increased and the ceiling effects reduced by administering PROMIS-43, which includes six items per domain, or by administering by computerized adaptive testing.
LEVEL OF EVIDENCE: Diagnostic Test or Criteria, level III.
PMID:34284470 | PMC:PMC9118559 | DOI:10.1097/TA.0000000000003365
J Patient Rep Outcomes. 2021 Jul 17;5(1):59. doi: 10.1186/s41687-021-00335-9.
ABSTRACT
BACKGROUND: The Satisfaction with Life Scale (SWLS) is a widely used measure of subjective well-being. Recent evidence indicates the fifth item of the scale reduces the reliability of the scale and is inappropriate for use in traumatic injury populations. The purpose of this study was to develop a linking procedure between the five-item version of the SWLS and a modified four-item version, which removes the problematic item, for use in Spinal Cord (SCI), Traumatic Brain (TBI), and Burn Injury populations.
METHODS: Proration (i.e. adding the mean of the four items to their total) was identified as a potential linking solution that could be easily implemented in clinical or research settings. The validity of the proration approach was evaluated by examining mean differences, cross group classification by SWLS category, score correlations, the intraclass correlation coefficient, and visual inspection of Bland-Altman plots in a large sample of SCI, TBI, and Burn Injury survivors who were participants in the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) Model Systems' National Databases.
RESULTS: A total of 17,897 (SCI n = 8566, TBI n = 7941, and Burn n = 1390) participants were included in this study. SWLS scores ranged from 5 to 35, and the average score difference between directly derived and prorated scores was 0.39 points. A large majority of the sample (93%) had score differences of < 4 points (i.e. approximately 0.5 SD). The correlation between the prorated and directly derived scores was very high (r = 0.97) and the ICC value indicated excellent reliability (ICC = 0.97).
CONCLUSIONS: This study provides a valid scoring approach for researchers or clinicians who don't want to lose continuity with previously collected data but prefer to switch to the modified four-item version of the SWLS. Clear guidance is provided for traumatic injury researchers or clinicians on how to implement the proration scoring approach.
PMID:34273011 | PMC:PMC8286208 | DOI:10.1186/s41687-021-00335-9
J Burn Care Res. 2021 Nov 24;42(6):1067-1075. doi: 10.1093/jbcr/irab104.
ABSTRACT
Pediatric burn injuries can alter the trajectory of the survivor's entire life. Patient-centered outcome measures are helpful to assess unique physical and psychosocial needs and long-term recovery. This study aimed to develop a conceptual framework to measure pediatric burn outcomes in survivors aged 5 to 12 years as a part of the School-Aged Life Impact Burn Recovery Evaluation Computer Adaptive Test (SA-LIBRE5-12 CAT) development. This study conducted a systematic literature review guided by the WHO International Classification of Functioning-Child and Youth and domains in the American Burn Association/Shriners Hospitals for Children Burn Outcomes Questionnaire5-18. Interviews with eight parents and seven clinicians were conducted to identify important domains in child recovery. One clinician focus group with four clinicians was completed to identify gaps in the preliminary framework, and semiweekly expert consensus meetings were conducted with three experts to solidify the framework. Qualitative data were analyzed by grounded theory methodology. Three major thematic outcome domains emerged: 1) Physical Functioning: fine motor and upper extremity, gross motor and lower extremity, pain, skin symptoms, sleep and fatigue, and physical resilience; 2) Psychological Functioning: cognitive, behavioral, emotional, resilience, and body image; and 3) Family and Social Functioning: family relationships, and parental satisfaction, school, peer relations, and community participation. The framework will be used to develop item banks for a CAT-based assessment of school-aged children's health and developmental outcomes, which will be designed for clinical and research use to optimize interventions, personalize care, and improve long-term health outcomes for burned children.
PMID:34228121 | PMC:PMC8760860 | DOI:10.1093/jbcr/irab104
J Burn Care Res. 2021 Nov 24;42(6):1110-1119. doi: 10.1093/jbcr/irab125.
ABSTRACT
People living with burn injury often report temperature sensitivity. However, its epidemiology and associations with health-related quality of life (HRQOL) are unknown. We aimed to characterize temperature sensitivity and determine its impact on HRQOL to inform patient education after recovery from burn injury. We used the multicenter, longitudinal Burn Model System National Database to assess temperature sensitivity at 6, 12, and 24 months after burn injury. Chi-square and Kruskal-Wallis tests determined differences in patient and injury characteristics. Multivariable, multilevel generalized linear regression models determined the association of temperature sensitivity with Satisfaction with Life (SWL) scale scores and Veterans RAND 12 (VR-12) physical and mental health summary component (MCS) scores. The cohort comprised 637 participants. Two thirds (66%) experienced temperature sensitivity. They had larger burns (12% TBSA, interquartile range [IQR] 4-30 vs 5% TBSA, IQR 2-15; P < .0001), required more grafting (5% TBSA, IQR 1-19 vs 2% TBSA, IQR 0-6; P < .0001), and had higher intensity of pruritus at discharge (11% severe vs 5% severe; P = .002). After adjusting for confounding variables, temperature sensitivity was strongly associated with lower SWL (odds ratio [OR] -3.2, 95% confidence interval [CI] -5.2, -1.1) and MCS (OR -4.0, 95% CI -6.9, -1.2) at 6 months. Temperature sensitivity decreased over time (43% at discharge, 4% at 24 months) and was not associated with poorer HRQOL at 12 and 24 months. Temperature sensitivity is common after burn injury and associated with worse SWL and MCS during the first year after injury. However, temperature sensitivity seems to improve and be less intrusive over time.
PMID:34212194 | PMC:PMC8633136 | DOI:10.1093/jbcr/irab125
J Am Med Dir Assoc. 2021 Dec;22(12):2461-2467. doi: 10.1016/j.jamda.2021.03.033. Epub 2021 May 11.
ABSTRACT
OBJECTIVES: To quantify the rate of readmission from inpatient rehabilitation facilities (IRFs) to acute care hospitals (ACHs) during the first 30 days of rehabilitation stay. To measure variation in 30-day readmission rate across IRFs, and the extent that patient and facility characteristics contribute to this variation.
DESIGN: Retrospective analysis of an administrative database.
SETTING AND PARTICIPANTS: Adult IRF discharges from 944 US IRFs captured in the Uniform Data System for Medical Rehabilitation database between October 1, 2015 and December 31, 2017.
METHODS: Multilevel logistic regression was used to calculate adjusted rates of readmission within 30 days of IRF admission and examine variation in IRF readmission rates, using patient and facility-level variables as predictors.
RESULTS: There were a total of 104,303 ACH readmissions out of a total of 1,102,785 IRFs discharges. The range of 30-day readmission rates to ACHs was 0.0%‒28.9% (mean = 8.7%, standard deviation = 4.4%). The adjusted readmission rate variation narrowed to 2.8%‒17.5% (mean = 8.7%, standard deviation = 1.8%). Twelve patient-level and 3 facility-level factors were significantly associated with 30-day readmission from IRF to ACH. A total of 82.4% of the variance in 30-day readmission rate was attributable to the model predictors.
CONCLUSIONS AND IMPLICATIONS: Fifteen patient and facility factors were significantly associated with 30-day readmission from IRF to ACH and explained the majority of readmission variance. Most of these factors are nonmodifiable from the IRF perspective. These findings highlight that adjusting for these factors is important when comparing readmission rates between IRFs.
PMID:33984292 | PMC:PMC8581059 | DOI:10.1016/j.jamda.2021.03.033
Burns. 2022 Feb;48(1):40-50. doi: 10.1016/j.burns.2021.04.015. Epub 2021 Apr 20.
ABSTRACT
INTRODUCTION: Facial burns account for persistent differences in psychosocial functioning in adult burn survivors. Although adolescent burn survivors experience myriad chronic sequelae, little is known about the effect of facial injuries. This study examines differences in long-term outcomes with and without head and neck involvement.
METHODS: Data collected for 392 burn survivors between 14-17.9 years of age from the Burn Model System National Database (2006-2015) were analyzed. Comparisons were made between two groups based on presence of a head and neck burn (H&N) using the following patient reported outcome measures: Satisfaction with Appearance Scale, Satisfaction with Life Scale, Community Integration Questionnaire, and Short Form-12 Health Survey at 6, 12, and 24 months after injury. Regression analyses were used to assess association between outcome measures and H&N group at 12-months.
RESULTS: The H&N group had more extensive burns, had longer hospital stays, were more likely to be burned by fire/flame and were more likely to be Hispanic compared to the non-H&N group. Regression analysis found that H&N burn status was associated with worse SWAP scores. No significant associations were found between H&N burn status and other outcome measures.
CONCLUSIONS: Adolescents with H&N burn status showed significantly worse satisfaction with appearance at 12-months after injury. Future research should examine interventions to help improve body image and coping for adolescent burn survivors with head and neck burns.
PMID:33975762 | PMC:PMC8526620 | DOI:10.1016/j.burns.2021.04.015
PM R. 2022 Apr;14(4):452-461. doi: 10.1002/pmrj.12618. Epub 2021 Jun 22.
ABSTRACT
INTRODUCTION: Representativeness of research populations impacts the ability to extrapolate findings. The Burn Model System (BMS) National Database is one of the largest prospective, longitudinal, multi-center research repositories collecting patient-reported outcomes after burn injury.
OBJECTIVE: To assess if the BMS Database is representative of the population that is eligible to participate.
DESIGN: Data on adult burn survivors who were eligible for the BMS Database from 2015 to 2019 were analyzed.
SETTING: Not applicable.
PARTICIPANTS: Burn survivors treated at BMS centers meeting eligibility criteria for the BMS Database. Eligibility for the database is based on burn size and receipt of autografting surgery.
INTERVENTIONS: Not applicable.
MAIN OUTCOME MEASURE(S): Race, ethnicity, gender, and age were compared between individuals who did and did not enroll. Regression analysis examined the correlation between demographic characteristics and study enrollment. Additional regression analysis examined the association between enrollment and the intersection of race, ethnicity, and gender.
RESULTS: A total of 982 adult burn survivors were eligible for the BMS database during the study period. Of those who were eligible, 72.1% Enrolled and 27.9% were Not Enrolled. The Enrolled group included more female and more younger survivors compared to the Not Enrolled group. In regression analyses, Black/African American burn survivors were less likely and individuals identifying as female were more likely to enroll in the BMS Database. Furthermore, White men and women were more likely to enroll compared to Black/African American men and women, and non-Hispanic/Latino men were more likely to enroll compared to Hispanic/Latino men.
CONCLUSIONS: This study found differences in BMS Database enrollment by race, ethnicity, and gender. Further research is warranted to investigate causes for the disparities found in this study. In addition, strategies are needed to improve enrollment to ensure future representativeness.
PMID:33886159 | PMC:PMC8531153 | DOI:10.1002/pmrj.12618
Burns. 2021 Nov;47(7):1511-1524. doi: 10.1016/j.burns.2021.02.010. Epub 2021 Feb 25.
ABSTRACT
Modern, reliable, and valid outcome measures are essential to understanding the health needs of young children with burn injuries. Burn-specific and age-appropriate legacy assessment tools exist for this population but are hindered by the limitations of existing paper-based instruments. The purpose of this study was to develop item pools comprised of questions appropriate for children aged 1-5 with burn injuries. Item development was based on a framework provided by previous work to develop the Preschool Life Impact Burn Recovery Evaluation (LIBRE) Conceptual Model. The Preschool LIBRE Conceptual Model work established four sub-domains of functioning for children with burns aged 1-5. Item development involved a systematic literature review, a qualitative item review process with clinical experts, and parent cognitive interviews. Four item pools were established: (1) communication and language development; (2) physical functioning; (3) psychological functioning and (4) social functioning for preschool-aged children with burn injuries. We selected and refined candidate items, recall periods, survey instructions, and response option choices through clinical and parental feedback during the qualitative review and cognitive interview processes. Item pools are currently being field-tested as part of the process to calibrate and validate the Preschool1-5 LIBRE Computer Adaptive Test (CAT) Profile.
PMID:33832799 | PMC:PMC8711655 | DOI:10.1016/j.burns.2021.02.010
PLoS One. 2021 Mar 31;16(3):e0248824. doi: 10.1371/journal.pone.0248824. eCollection 2021.
ABSTRACT
OBJECTIVE: To characterize the functional impairments of a cohort of patients undergoing inpatient rehabilitation after surviving severe COVID-19 illness, in order to better understand the ongoing needs of this patient population.
METHODS: This study consisted of a retrospective chart review of consecutive patients hospitalized for COVID-19 and admitted to a regional inpatient rehabilitation hospital from April 29th to May 22nd, 2020. Patient demographics, clinical characteristics and complications from acute hospitalization were examined. Measures of fall risk (Berg Balance Scale), endurance (6 Minute Walk Test), gait speed (10 Meter Walk Test), mobility (transfer and ambulation independence), cognition, speech and swallowing (American Speech and Hearing Association National Outcomes Measurement System Functional Communication Measures) were assessed at rehabilitation admission and discharge.
RESULTS: The study population included 29 patients and was 70% male, 58.6% white and with a mean age of 59.5. The mean length of acute hospitalization was 32.2 days with a mean of 18.7 days intubated. Patients spent a mean of 16.7 days in inpatient rehabilitation and 90% were discharged home. Patients demonstrated significant improvement from admission to discharge in measures of fall risk, endurance, gait speed, mobility, cognition, speech and swallowing, (p< 0.05). At discharge, a significant portion of the population continued to deficits in cognition (attention 37%; memory 28%; problem solving 28%), balance (55%) and gait speed (97%).
CONCLUSION: Patients admitted to inpatient rehabilitation after hospitalization with COVID-19 demonstrated deficits in mobility, cognition, speech and swallowing at admission and improved significantly in all of these domains by discharge. However, a significant number of patients exhibited residual deficits at discharge highlighting the post-acute care needs of this patient population.
PMID:33788876 | PMC:PMC8011729 | DOI:10.1371/journal.pone.0248824
PM R. 2022 Apr;14(4):462-471. doi: 10.1002/pmrj.12589. Epub 2021 Jun 9.
ABSTRACT
BACKGROUND: Comorbidity indices have been used to represent the overall medical complexity of patient populations in clinical research; however, it is not known how well they capture the comorbidities of patients with a stroke or brain injury admitted to inpatient rehabilitation facilities (IRFs).
OBJECTIVE: To determine how well commonly used comorbidity indices capture the comorbidities of patients admitted to IRFs after a stroke or brain injury.
DESIGN: Cross-sectional, retrospective study.
SETTING: IRFs nationwide.
PARTICIPANTS: Adults from four impairment groups: (1) hemorrhagic stroke, (2) ischemic stroke, (3) nontraumatic brain injury (NTBI), and (4) traumatic brain injury (TBI).
MAIN OUTCOME MEASURES: International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes were extracted from the Uniform Data System for Medical Rehabilitation (UDSMR) for IRF discharges from October 1, 2015 to December 31, 2017. The percentage of discharges captured by Deyo-Charlson, Elixhauser, and Centers for Medicare and Medicaid Services (CMS) tiers was determined, as was the percentage of comorbidities captured. These measures were also compared with respect to their ability to capture chronic medical complexity by examining the percentage of codes captured after removal of codes deemed to represent hospital complications or sequela of the admission diagnosis.
RESULTS: The percentage of discharges without at least one ICD-10-CM code captured by any index ranged from 0.3%-3.8%. The percentage of comorbidities with a prevalence exceeding 1% captured by at least one index ranged from 37.1%-43.6%. Chronic comorbidities were most likely to be captured by Elixhauser (40.7%-44.4%), followed by Deyo-Charlson (7.8%-9.6%), then CMS tiers (4.5%-6.9%). Existing comorbidity measures capture most IRF discharges related to a brain injury or stroke, whereas most medical comorbidities escape representation. Several common, functionally relevant diagnoses were not captured.
CONCLUSION: The use of comorbidity indices in the IRF neurologic injury population should account for the fact that these measures miss several common, important comorbidities.
PMID:33728804 | DOI:10.1002/pmrj.12589
Ann Surg. 2022 Dec 1;276(6):1056-1062. doi: 10.1097/SLA.0000000000004703. Epub 2020 Dec 18.
ABSTRACT
OBJECTIVE: To assess the association of burn size and community participation as measured by the LIBRE Profile.
SUMMARY OF BACKGROUND DATA: Burn size is an established clinical predictor of survival after burn injury. It is often a factor in guiding decisions surrounding early medical interventions; however, literature is inconclusive on its relationship to quality of life outcomes.
METHODS: This is a secondary data analysis of a cross-sectional survey of adult burn survivors. Self-reported data were collected between October 2014 and December 2015 from 601 burn survivors aged ≥18 years with ≥5% total body surface area (TBSA) or burns to critical areas. Sociodemographic characteristics were compared between participants with small burns (≤40% TBSA burned) and large burns (>40% TBSA burned). Ordinary least squares regression models examined associations between burn size and LIBRE Profile scale scores with adjustments for sex, current work status, burns to critical areas, and time since burn injury.
RESULTS: The analytic sample comprised 562 participants with data available for burn size. 42% of respondents had large burns (>40% TBSA burned) and 58% reported smaller burns (TBSA ≤40%). In adjusted regression models, patients with large burns tended to score lower on the Social Activities and Work & Employment scales ( P < 0.05) and higher on the Family & Friends scale ( P < 0.05). Participants with burns >40% TBSA scored lower for several individual items in the Social Activities scale and one item in the Work & Employment scale ( P < 0.05).
CONCLUSIONS: Increasing burn size was found to be negatively associated with selected items of Work & Employment and Social Activities, but positively associated with aspects of Family & Friend Relationships. Future longitudinal studies are necessary to assess and understand the long-term social impact of burn injuries on adult populations.
PMID:33351466 | PMC:PMC8265012 | DOI:10.1097/SLA.0000000000004703
Burns. 2021 May;47(3):525-537. doi: 10.1016/j.burns.2020.06.005. Epub 2020 Jun 20.
ABSTRACT
Burn survivors experience myriad associated symptoms such as pain, pruritus, fatigue, impaired motor strength, post-traumatic stress, depression, anxiety, and sleep disturbance. Many of these symptoms are common and remain chronic, despite current standard of care. One potential novel intervention to target these post burn symptoms is transcranial direct current stimulation (tDCS). tDCS is a non-invasive brain stimulation (NIBS) technique that modulates neural excitability of a specific target or neural network. The aim of this work is to review the neural circuits of the aforementioned clinical sequelae associated with burn injuries and to provide a scientific rationale for specific NIBS targets that can potentially treat these conditions. We ran a systematic review, following the PRISMA statement, of tDCS effects on burn symptoms. Only three studies matched our criteria. One was a feasibility study assessing cortical plasticity in chronic neuropathic pain following burn injury, one looked at the effects of tDCS to reduce pain anxiety during burn wound care, and one assessed the effects of tDCS to manage pain and pruritus in burn survivors. Current literature on NIBS in burn remains limited, only a few trials have been conducted. Based on our review and results in other populations suffering from similar symptoms as patients with burn injuries, three main areas were selected: the prefrontal region, the parietal area and the motor cortex. Based on the importance of the prefrontal cortex in the emotional component of pain and its implication in various psychosocial symptoms, targeting this region may represent the most promising target. Our review of the neural circuitry involved in post burn symptoms and suggested targeted areas for stimulation provide a spring board for future study initiatives.
PMID:33293156 | PMC:PMC8685961 | DOI:10.1016/j.burns.2020.06.005
Burns. 2021 Feb;47(1):250-251. doi: 10.1016/j.burns.2020.04.018. Epub 2020 Apr 24.
NO ABSTRACT
PMID:33280957 | PMC:PMC7180154 | DOI:10.1016/j.burns.2020.04.018
J Burn Care Res. 2021 May 7;42(3):425-433. doi: 10.1093/jbcr/iraa169.
ABSTRACT
Contractures can complicate burn recovery. There are limited studies examining the prevalence of contractures following burns in pediatrics. This study investigates contracture outcomes by location, injury, severity, length of stay, and developmental stage. Data were obtained from the Burn Model System between 1994 and 2003. All patients younger than the age of 18 with at least one joint contracture at hospital discharge were included. Sixteen areas of impaired movement from the shoulder, elbow, wrist, hand, hip, knee, and ankle joints were examined. Analysis of variance was used to assess the association between contracture severity, burn size, and length of stay. Age groupings were evaluated for developmental patterns. A P value of less than .05 was considered statistically significant. Data from 225 patients yielded 1597 contractures (758 in the hand) with a mean of 7.1 contractures (median 4) per patient. Mean contracture severity ranged from 17% (elbow extension) to 41% (ankle plantarflexion) loss of movement. Statistically significant associations were found between active range of motion loss and burn size, length of stay, and age groupings. The data illustrate quantitative assessment of burn contractures in pediatric patients at discharge in a multicenter database. Size of injury correlates with range of motion loss for many joint motions, reflecting the anticipated morbidity of contracture for pediatric burn survivors. These results serve as a potential reference for range of motion outcomes in the pediatric burn population, which could serve as a comparison for local practices, quality improvement measures, and future research.
PMID:33247583 | PMC:PMC8344380 | DOI:10.1093/jbcr/iraa169
Burns. 2021 Feb;47(1):42-51. doi: 10.1016/j.burns.2020.09.007. Epub 2020 Oct 4.
ABSTRACT
OBJECTIVE: Despite improved mortality rates after burn injury, many patients face significant long-term physical and psychosocial disabilities. We aimed to determine whether commonly used mortality prognostication scores predict long-term, health-related quality of life after burn injury. By doing so, we might add evidence to support goals of care discussions and facilitate shared decision-making efforts in the hours and days after a life-changing injury.
METHODS: We used the multicenter National Institute of Disability, Independent Living and Rehabilitation Research Burn Model System database (1994-2019) to analyze SF-12 physical (PCS) and mental component (MCS) scores among survivors one year after major burn injury. Ninety percent of the observations were randomly assigned to a model development dataset. Multilevel, mixed-effects, linear regression models determined the relationship between revised Baux and Ryan Scores and SF-12 measures. Additionally, we tested a model with disaggregated independent and other covariates easily obtained around the time of index admission: age, sex, race, burn size, inhalation injury. Residuals from the remaining 10% of observations in the validation dataset were examined.
RESULTS: The analysis included 1606 respondents (median age 42 years, IQR 28-53 years; 70% male). Median burn size was 16% TBSA (IQR 6-30) and 13% of respondents sustained inhalation injury. Higher revised Baux and Ryan Scores and age, burn size, and inhalation injury were significantly correlated with lower PCS, but were not correlated with MCS. Female sex, black race, burn size, and inhalation injury correlated with lower MCS. All models poorly explained the variance in SF-12 scores (adjusted r2 0.01-0.12).
CONCLUSION: Higher revised Baux and Ryan Scores negatively correlated with long-term physical health, but not mental health, after burn injury. Regardless, the models poorly explained the variance in SF-12 scores one year after injury. More accurate models are needed to predict long-term, health-related quality of life and support shared decision-making during acute burn care.
PMID:33092898 | PMC:PMC7533049 | DOI:10.1016/j.burns.2020.09.007
iScience. 2020 Nov 20;23(11):101659. doi: 10.1016/j.isci.2020.101659. Epub 2020 Oct 7.
ABSTRACT
Severe trauma predisposes patients to multiple independent infection episodes (MIIEs), leading to augmented morbidity and mortality. We developed a method to identify increased MIIE risk before clinical signs appear, which is fundamentally different from existing approaches entailing infections' detection after their establishment. Applying machine learning algorithms to genome-wide transcriptome data from 128 adult blunt trauma patients' (42 MIIE cases and 85 non-cases) leukocytes collected ≤48 hr of injury and ≥3 days before any infection, we constructed a 15-transcript and a 26-transcript multi-biomarker panel model with the least absolute shrinkage and selection operator (LASSO) and Elastic Net, respectively, which accurately predicted MIIE (Area Under Receiver Operating Characteristics Curve [AUROC] [95% confidence intervals, CI]: 0.90 [0.84-0.96] and 0.92 [0.86-0.96]) and significantly outperformed clinical models. Gene Ontology and network analyses found various pathways to be relevant. External validation found our model to be generalizable. Our unique precision medicine approach can be applied to a wide range of patient populations and outcomes.
PMID:33047099 | PMC:PMC7539926 | DOI:10.1016/j.isci.2020.101659
PM R. 2021 Jan;13(1):81-86. doi: 10.1002/pmrj.12506. Epub 2020 Dec 25.
NO ABSTRACT
PMID:33025674 | PMC:PMC7675300 | DOI:10.1002/pmrj.12506
J Burn Care Res. 2021 May 7;42(3):398-407. doi: 10.1093/jbcr/iraa161.
ABSTRACT
The Burn Model System (BMS) program of research has been funded since 1993 by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR). The overarching aim of this program is to improve outcomes and quality of life for people with burns in the areas of health and function, employment, and community living and participation. This review reports on BMS contributions that have affected the lives of individuals with a significant burn injury using case reports to associate BMS contributions with recovery. In January 2020, current BMS grantee researchers assessed peer-reviewed BMS publications from 1994 to 2020. Using case report methodology, contributions were linked to three individuals treated at one of the four Burn Model System institutions. With over 25 years of NIDILRR funding, unique BMS contributions to patient recovery were identified and categorized into one of several domains: treatment, assessment measures, sequelae, peer support, employment, and long-term functional outcomes. A second review for significant results of BMS research that add to the understanding of burn injury, pathophysiology, and recovery research was identified and categorized as injury recovery research. The case study participants featured in this review identified select NIDILRR research contributions as having direct, personal benefit to their recovery. The knowledge generation and clinical innovation that this research program has contributed to our collective understanding of recovery after burn injury is considerable. Using case study methodology with three adult burn survivors, we highlight the impact and individual significance of program findings and reinforce the recognition that the value of any clinical research must have relevance to the lives of the study population.
PMID:32971531 | PMC:PMC10044562 | DOI:10.1093/jbcr/iraa161
PLoS One. 2020 Sep 23;15(9):e0239556. doi: 10.1371/journal.pone.0239556. eCollection 2020.
ABSTRACT
INTRODUCTION: Inhalation injuries carry significant acute care burden including prolonged ventilator days and length of stay. However, few studies have examined post-acute outcomes of inhalation injury survivors. This study compares the long-term outcomes of burn survivors with and without inhalation injury.
METHODS: Data collected by the Burn Model System National Database from 1993 to 2019 were analyzed. Demographic and clinical characteristics for adult burn survivors with and without inhalation injury were examined. Outcomes included employment status, Short Form-12/Veterans Rand-12 Physical Composite Score (SF-12/VR-12 PCS), Short Form-12/Veterans Rand-12 Mental Composite Score (SF-12/VR-12 MCS), and Satisfaction With Life Scale (SWLS) at 24 months post-injury. Regression models were used to assess the impacts of sociodemographic and clinical covariates on long-term outcome measures. All models controlled for demographic and clinical characteristics.
RESULTS: Data from 1,871 individuals were analyzed (208 with inhalation injury; 1,663 without inhalation injury). The inhalation injury population had a median age of 40.1 years, 68.8% were male, and 69% were White, non-Hispanic. Individuals that sustained an inhalation injury had larger burn size, more operations, and longer lengths of hospital stay (p<0.001). Individuals with inhalation injury were less likely to be employed at 24 months post-injury compared to survivors without inhalation injury (OR = 0.63, p = 0.028). There were no significant differences in PCS, MCS, or SWLS scores between groups in adjusted regression analyses.
CONCLUSIONS: Burn survivors with inhalation injury were significantly less likely to be employed at 24 months post-injury compared to survivors without inhalation injury. However, other health-related quality of life outcomes were similar between groups. This study suggests distinct long-term outcomes in adult burn survivors with inhalation injury which may inform future resource allocation and treatment paradigms.
PMID:32966317 | PMC:PMC7511001 | DOI:10.1371/journal.pone.0239556
Burns. 2020 Nov;46(7):1556-1564. doi: 10.1016/j.burns.2020.01.003. Epub 2020 Sep 15.
ABSTRACT
BACKGROUND: Engaging in healthy sexual activity and romantic relationships are important but often neglected areas of post-burn rehabilitation. The degree to which persons with burn injuries engage in sexual activity and romantic relationships is not well understood. This study examined demographic and clinical characteristics predicting engagement in sexual activity and romantic relationships in a sample of adult burn survivors compared to a general United States sample.
METHODS: Data for the adult burn survivor sample were from 601 adult burn survivors who participated in field-testing for the calibration of the Life Impact Burn Recovery Evaluation (LIBRE) Profile, a burn-specific instrument assessing social participation on six scales including sexual activity and romantic relationships. Comparison data were obtained from a general population sample of 2000 adults through sample matching. Demographic predictors of sexual activity and romantic relationship status were examined in each sample using modified Poisson regression analyses. Clinical predictors of engaging in sexual activity and romantic relationships were also examined in the LIBRE sample.
RESULTS: Participants were slightly more likely to report being sexually active in the adult burn survivor sample than in the general sample (65% vs. 57%, p < 0.01). There was not a significant difference in romantic relationship status between the two samples (64% vs. 62%, p = 0.31). In multivariable regression analyses, men in both samples were more likely to report being in a sexual relationship (RR in LIBRE sample = 1.23, 95% CI 1.08-1.39; RR in general sample = 1.10, 95% CI 1.02-1.18). Participants in both samples who were not working were less likely to report being sexually active or in a romantic relationship (RRs ranging from 0.73 to 0.83, p < 0.05 for all estimates). In the adult burn survivor sample, respondents with hand burns were more likely to report being sexually active and in a romantic relationship (RR = 1.16, 95% CI 1.01-1.33). Time since burn injury, burn size, and burns to other critical areas were not significantly associated with either outcome in adjusted analyses.
CONCLUSIONS: The likelihood of engaging in sexual activity and romantic relationships is similar among adult burn survivors and the comparison group representing a general United States sample of adults. Further research addressing sexual activity and romantic relationships after burn injuries will help to foster better patient-clinician dialogue, pinpoint barriers, design interventions, and allocate appropriate resources.
PMID:32948357 | PMC:PMC8279809 | DOI:10.1016/j.burns.2020.01.003
J Burn Care Res. 2020 Nov 30;41(6):1152-1164. doi: 10.1093/jbcr/iraa120.
NO ABSTRACT
PMID:32885252 | PMC:PMC7703674 | DOI:10.1093/jbcr/iraa120
J Burn Care Res. 2020 Nov 30;41(6):1129-1151. doi: 10.1093/jbcr/iraa119.
ABSTRACT
The ABA pain guidelines were developed 14 years ago and have not been revised despite evolution in the practice of burn care. A sub-committee of the American Burn Association's Committee on the Organization and Delivery of Burn Care was created to revise the adult pain guidelines. A MEDLINE search of English-language publications from 1968 to 2018 was conducted using the keywords "burn pain," "treatment," and "assessment." Selected references were also used from the greater pain literature. Studies were graded by two members of the committee using Oxford Centre for Evidence-based Medicine-Levels of Evidence. We then met as a group to determine expert consensus on a variety of topics related to treating pain in burn patients. Finally, we assessed gaps in the current knowledge and determined research questions that would aid in providing better recommendations for optimal pain management of the burn patient. The literature search produced 189 papers, 95 were found to be relevant to the assessment and treatment of burn pain. From the greater pain literature 151 references were included, totaling 246 papers being analyzed. Following this literature review, a meeting to establish expert consensus was held and 20 guidelines established in the areas of pain assessment, opioid medications, nonopioid medications, regional anesthesia, and nonpharmacologic treatments. There is increasing research on pain management modalities, but available studies are inadequate to create a true standard of care. We call for more burn specific research into modalities for burn pain control as well as research on multimodal pain control.
PMID:32885244 | PMC:PMC7703676 | DOI:10.1093/jbcr/iraa119
J Burn Care Res. 2021 Mar 4;42(2):212-219. doi: 10.1093/jbcr/iraa133.
ABSTRACT
Pruritus is a commonly reported symptom after burn injury. Valid and reliable scales to measure itch in pediatric burn survivors are important for treatment and epidemiological studies. This study sought to develop psychometrically sound, publicly available self- and proxy-report measures of itch for use in pediatric burn survivors suitable for use in research and clinical practice. A panel of burn experts developed a definition of itch interference and a set of parallel self- and proxy-report candidate items that covered important activities affected by itch. Candidate items were evaluated in cognitive interviews with pediatric burn survivors (n = 4) and proxies (n = 2). Items were translated to Spanish and administered in both English and Spanish to a sample (N = 264) of pediatric burn survivors and/or their proxy enrolled in the Burn Model System (BMS) longitudinal database. The mean age of the pediatric sample was 13 years and average time since burn 5 years. The final itch interference measures each included 5 parallel items calibrated using a one-parameter graded response item response theory model, with a mean of 50 representing the average itch interference of the sample. Reliability of the scores is excellent between the mean and two standard deviations above. Initial analyses provide support for validity of the score. Concordance between the self- and proxy-report scores was moderate (ICC = 0.68). The results support the reliability and validity of the itch scale in children and youth with burn injury. The new BMS Pediatric Itch Interference scales are freely and publicly available at https://burndata.washington.edu/itch.
PMID:32810205 | PMC:PMC9165661 | DOI:10.1093/jbcr/iraa133
PM R. 2021 Jul;13(7):666-673. doi: 10.1002/pmrj.12465. Epub 2020 Oct 7.
ABSTRACT
BACKGROUND: To date, no large population studies compare left and right middle cerebral artery (MCA) strokes and corresponding patient performance in acute rehabilitation as measured by the Functional Independence Measure (FIM).
OBJECTIVE: To compare granular performance data using the six FIM subcategories between left and right MCA territory strokes. This may foster development of individualized rehabilitation programs and affect rehabilitation policy based on phenotypic variations.
DESIGN: Retrospective cohort study.
SETTING: Inpatient rehabilitation facilities, using Uniform Data System for Medical Rehabilitation data from 2015 to 2017.
PATIENTS: Individuals with MCA strokes admitted to inpatient rehabilitation facilities (n = 38 812).
MAIN OUTCOME MEASURES: Mean FIM efficiency and FIM gain within the six FIM subcategories (self-care, sphincter control, transfers, locomotion, communication, and social cognition) were compared between left and right MCA strokes. All were stratified by admission FIM severity categories (<40, 40-80, >80). The study also examined length of stay and percentage discharged to home.
RESULTS: Mean FIM efficiency was significantly higher for left MCA strokes compared to right MCA strokes. Left MCA strokes with admission FIM <40 and 40-80 had significantly higher FIM efficiencies within the majority of FIM subcategories. However, left and right MCA strokes with admission FIM > 80 did not display any significant differences. Overall, patients with left MCA strokes were discharged to home at a significantly higher percentage. Patients with left MCA strokes with admission FIM 40-80 had on average a 2-day shorter length of stay than those with right MCA strokes.
CONCLUSIONS: Overall, patients with left MCA ischemic strokes had shorter length of stays, higher FIM efficiencies, and larger FIM gains than those with right MCA strokes. These results allow clinicians to counsel patients regarding functional gains based on diagnosis and to tailor rehabilitation programs to impairments encountered in left and right MCA territories. Including laterality of stroke and admission functional status would also improve algorithms for determining reimbursement.
PMID:32772438 | DOI:10.1002/pmrj.12465
Pain Rep. 2020 Jul 20;5(4):e828. doi: 10.1097/PR9.0000000000000828. eCollection 2020 Jul-Aug.
ABSTRACT
Opioid consumption for those in comprehensive inpatient rehabilitation units is high because of the complexity of their injuries. Notably, pain in rehabilitation leads to worsened clinical outcomes because of maladaptive behaviors and poor engagement during therapies. It is critical to developing evidence-based pharmacobehavioral interventions. Based on principles of classical conditioning, conditioning open-label placebo (COLP) is a promising approach for reducing opioid use in comprehensive inpatient rehabilitation, and this technique takes advantage of the possibility of association learning and opioid pharmacology to promote evoked placebo-driven analgesia.
OBJECTIVES: In this brief report, we evaluate the feasibility of COLP as a pharmacobehavioral intervention to decrease total opioid consumption in patients with pain hospitalized at Spaulding Rehabilitation Hospital.
METHODS: Inpatients with spinal cord injury and polytrauma (n = 20) with moderate to severe pain were randomized to receive COLP (n = 10) or treatment-as-usual for 6 consecutive days. Opioid utilization was measured by morphine equivalents using the morphine equivalent dose conversion; pain severity was assessed using the numerical visual analog scale.
RESULTS: Conditioning open-label placebo significantly reduced total opioid consumption by the end of the intervention period (P ≤ 0.001). Pain reduction was also significant for the COLP group (P = 0.005), whereas the treatment-as-usual group demonstrated a trend towards pain reduction (P = 0.05).
CONCLUSIONS: This study presents the first data in the use of a pharmacobehavioral intervention that capitalize on the benefits of open-label placebo and classical drug conditioning for opioid dose reduction in a population with moderate to severe pain exposed to intensive inpatient rehabilitation.
PMID:32766465 | PMC:PMC7373570 | DOI:10.1097/PR9.0000000000000828
Am J Phys Med Rehabil. 2020 Sep;99(9):787-788. doi: 10.1097/PHM.0000000000001512.
NO ABSTRACT
PMID:32576749 | DOI:10.1097/PHM.0000000000001512
J Burn Care Res. 2021 Feb 3;42(1):23-31. doi: 10.1093/jbcr/iraa100.
ABSTRACT
The Life Impact Burn Recovery Evaluation (LIBRE) Profile is a patient-reported outcome measure developed to assess social participation in adult burn survivors. This study identified numeric score cut-points that define different levels of social participation ability and described each level. An expert panel identified numeric score cut-points that distinguish different levels of social participation for the six LIBRE Profile domains. Methods employed an iterative, modified-Delphi approach, and bookmarking to review calibrated item banks. Analyses (using calibration sample data and repeated in a validation sample) examined means, SDs, and sample distributions for each level. Analyses of variance examined score differences between levels. The panel developed descriptions for each established level. Initial cut-points resulted in four levels for five domains (Social Activities, Social Interactions, Romantic Relationships, Sexual Relationships, and Work & Employment) and five levels for the sixth domain (Relationships with Family & Friends). Comparisons demonstrated significant differences between level mean scores for all domains (P < .05) except Relationships with Family & Friends. Based on follow-up surveys, Relationships with Family & Friends score cut-points were adjusted to identify four levels with significant score differences between all levels. Panelists reached consensus for level descriptions. Score cut-points and descriptions identify different levels of social participation, providing a relevant context for interpreting LIBRE Profile numeric scores. LIBRE Profile Social Participation levels will help clinicians and persons with burn injury interpret LIBRE Profile numeric scores and promote use of this important new assessment.
PMID:32556266 | PMC:PMC8265741 | DOI:10.1093/jbcr/iraa100
Arch Phys Med Rehabil. 2020 Oct;101(10):1731-1738. doi: 10.1016/j.apmr.2020.04.025. Epub 2020 May 27.
ABSTRACT
OBJECTIVE: To examine whether commonly used comorbidity indexes (Deyo-Charlson comorbidity index, Elixhauser comorbidity index, the Centers for Medicare and Medicaid Services [CMS] comorbidity tiers) capture comorbidities in the acute traumatic and nontraumatic SCI inpatient rehabilitation population.
DESIGN: Retrospective cross-sectional study.
PARTICIPANTS: Data were obtained from the Uniform Data System for Medical Rehabilitation from October 1, 2015 to December 31, 2017 for adults with spinal cord injury (SCI) (Medicare-established Impairment Group Codes 04.110-04.230, 14.1, 14.3). This study included SCI discharges (N=66,235) from 833 inpatient rehabilitation facilities.
MAIN OUTCOME MEASURES: International Classification of Diseases-10th Revision-Clinical Modifications (ICD-10-CM) codes were used to assess 3 comorbidity indexes (Deyo-Charlson comorbidity index, Elixhauser comorbidity index, CMS comorbidity tiers). The comorbidity codes that occurred with >1% frequency were reported. The percentages of discharges for which no comorbidities were captured by each comorbidity index were calculated.
RESULTS: Of the total study population, 39,285 (59.3%) were men and 11,476 (17.3%) were tetraplegic. The mean number of comorbidities was 14.7. There were 13,939 distinct ICD-10-CM comorbidity codes. There were 237 comorbidities that occurred with >1% frequency. The Deyo-Charlson comorbidity index, Elixhauser comorbidity index, and the CMS tiers did not capture comorbidities of 58.4% (95% confidence interval, 58.08%-58.84%), 29.4% (29.07%-29.76%), and 66.1% (65.73%-66.46%) of the discharges in our study, respectively, and 28.8% (28.42%-29.11%) of the discharges did not have any comorbidities captured by any of the comorbidity indexes.
CONCLUSION: Commonly used comorbidity indexes do not reflect the extent of comorbid disease in the SCI rehabilitation population. This work suggests that alternative measures may be needed to capture the complexity of this population.
PMID:32473110 | DOI:10.1016/j.apmr.2020.04.025
Anesth Analg. 2020 Aug;131(2):497-507. doi: 10.1213/ANE.0000000000004852.
ABSTRACT
BACKGROUND: Unanticipated hospital admission is regarded as a measure of adverse perioperative patient care. However, previously published studies for risk prediction after ambulatory procedures are sparse compared to those examining readmission after inpatient surgery. We aimed to evaluate the incidence and reasons for unplanned admission after ambulatory surgery and develop a prediction tool for preoperative risk assessment.
METHODS: This retrospective cohort study included adult patients undergoing ambulatory, noncardiac procedures under anesthesia care at 2 tertiary care centers in Massachusetts, United States, between 2007 and 2017 as well as all hospitals and ambulatory surgery centers in New York State, United States, in 2014. The primary outcome was unplanned hospital admission within 30 days after discharge. We created a prediction tool (the PREdicting admission after Outpatient Procedures [PREOP] score) using stepwise backward regression analysis to predict unplanned hospital admission, based on criteria used by the Centers for Medicare & Medicaid Services, within 30 days after surgery in the Massachusetts hospital network registry. Model predictors included patient demographics, comorbidities, and procedural factors. We validated the score externally in the New York state registry. Reasons for unplanned admission were assessed.
RESULTS: A total of 170,983 patients were included in the Massachusetts hospital network registry and 1,232,788 in the New York state registry. Among those, the observed rate of unplanned admission was 2.0% (3504) and 1.7% (20,622), respectively. The prediction model showed good discrimination in the training set with C-statistic of 0.77 (95% confidence interval [CI], 0.77-0.78) and satisfactory discrimination in the validation set with C-statistic of 0.71 (95% CI, 0.70-0.71). The risk of unplanned admission varied widely from 0.4% (95% CI, 0.3-0.4) among patients whose calculated PREOP scores were in the first percentile to 21.3% (95% CI, 20.0-22.5) among patients whose scores were in the 99th percentile. Predictions were well calibrated with an overall ratio of observed-to-expected events of 99.97% (95% CI, 96.3-103.6) in the training and 92.6% (95% CI, 88.8-96.4) in the external validation set. Unplanned admissions were most often related to malignancy, nonsurgical site infections, and surgical complications.
CONCLUSIONS: We present an instrument for prediction of unplanned 30-day admission after ambulatory procedures under anesthesia care validated in a statewide cohort comprising academic and nonacademic hospitals as well as ambulatory surgery centers. The instrument may be useful in identifying patients at high risk for 30-day unplanned hospital admission and may be used for benchmarking hospitals, ambulatory surgery centers, and practitioners.
PMID:32427660 | DOI:10.1213/ANE.0000000000004852
J Burn Care Res. 2020 Jul 3;41(4):770-779. doi: 10.1093/jbcr/iraa050.
ABSTRACT
Burn care remains among the most complex of the time-sensitive treatment interventions in medicine today. An enormous quantity of specialized resources are required to support the critical and complex modalities needed to meet the conventional standard of care for each patient with a critical burn injury. Because of these dependencies, a sudden surge of patients with critical burn injuries requiring immediate and prolonged care following a burn mass casualty incident (BMCI) will place immense stress on healthcare system assets, including supplies, space, and an experienced workforce (staff). Therefore, careful planning to maximize the efficient mobilization and rational use of burn care resources is essential to limit morbidity and mortality following a BMCI. The U.S. burn care profession is represented by the American Burn Association (ABA). This paper has been written by clinical experts and led by the ABA to provide further clarity regarding the capacity of the American healthcare system to absorb a surge of burn-injured patients. Furthermore, this paper intends to offer responders and clinicians evidence-based tools to guide their response and care efforts to maximize burn care capabilities based on realistic assumptions when confronted with a BMCI. This effort also aims to align recommendations in part with those of the Committee on Crisis Standards of Care for the Institute of Medicine, National Academies of Sciences. Their publication guided the work in this report, identified here as "conventional, contingency, and crisis standards of care." This paper also includes an update to the burn Triage Tables- Seriously Resource-Strained Situations (v.2).
PMID:32298453 | PMC:PMC7530540 | DOI:10.1093/jbcr/iraa050
J Burn Care Res. 2020 Sep 23;41(5):1052-1062. doi: 10.1093/jbcr/iraa038.
ABSTRACT
Existing burn center referral criteria were developed several years ago, and subsequent innovations in burn care have occurred. Coupled with frequent errors in the estimation of extent of burn injury and depth by referring providers, patients are both over and under-triaged when the existing criteria are used to support patient care decisions. In the absence of compelling clinical trial data on appropriate burn patient triage, we convened a multidisciplinary panel of experts to execute an iterative eDelphi consensus process to facilitate a revision. The eDelphi process panel consisted of n = 61 burn stakeholders and experts and progressed through four rounds before reaching consensus on key clinical domains. The major findings are that 1) burn center consultation is strongly recommended for all patients with deep partial-thickness or deeper burns ≥ 10% TBSA burned, for full-thickness burns ≥ 5% TBSA burned, for children and older adults with specific dressing and medical needs, and for special burn circumstances including electrical, chemical, and radiation injuries; 2) smaller burns are ideally followed in burn center outpatient settings as soon as possible after injury, preferably without delays of a week or more; 3) frostbite, Stevens-Johnson syndrome/TENS, and necrotizing soft-tissue infection patients benefit from burn center treatment; and 4) telemedicine and technological solutions are of likely benefit in achieving this standard. Unlike the original criteria, the revised consensus-based guidelines create a framework promoting communication so that triage and treatment are specifically tailored to individual patient characteristics, injury severity, geography, and the capabilities of referring institutions.
PMID:32123911 | PMC:PMC7510842 | DOI:10.1093/jbcr/iraa038
Burns. 2020 May;46(3):539-545. doi: 10.1016/j.burns.2020.02.001. Epub 2020 Feb 20.
ABSTRACT
INTRODUCTION: Despite many advances in burn care, the development of extremity contracture remains a common and vexing problem. Extremity contractures have been documented in up to one third of severely burned patients at discharge. However, little is known about the long-term impact of these contractures. The purpose of this study was to examine the association of extremity contractures with employment after burn injury.
METHODS: We obtained data from the Burn Model System database from 1994 to 2003. We included in the study cohort all adult patients who were working prior to injury and identified those discharged with and without a contracture in one of the major extremity joints (shoulder, elbow, wrist, hip, knee and ankle). We classified contracture severity according to mild, moderate and severe categories. We performed descriptive analyses and predictive modeling to identify injury and patient factors associated with return to work (RTW) at 6, 12, and 24 months.
RESULTS: A total of 1,203 participant records met criteria for study inclusion. Of these, 415 (35%) had developed a contracture at discharge; 9% mild, 12% moderate, and 14% severe. Among 801 (67%) participants who had complete data at 6 months after discharge, 70% of patients without contracture had returned to work compared to 45% of patients with contractures (p < 0.001). RTW increased at each subsequent follow-up time point for the contracture group, however, it remained significantly lower than in no-contracture group (both p < 0.01). In multivariable analyses, female sex, non-Caucasian ethnicity, larger burn size, alcohol abuse, number of in-hospital operations, amputation, and in-hospital complications were associated with a lower likelihood of employment. In adjusted analyses, discharge contracture was associated with a lower probability of RTW at all 3 time points, although its impact significantly diminished at 24 months.
CONCLUSIONS: This study indicates an association between discharge contracture and reduced employment 6, 12 and 24 months after burn injury. Among many other identified patient, injury, and hospitalization related factors that are barriers to RTW, the presence of a contracture at discharge adds a significant reintegration burden for working-age burn patients.
PMID:32088093 | PMC:PMC9201560 | DOI:10.1016/j.burns.2020.02.001
Ann Plast Surg. 2020 Jun;84(6):644-650. doi: 10.1097/SAP.0000000000002287.
ABSTRACT
BACKGROUND: Geography is an important yet underexplored factor that may influence the care and outcomes of burn survivors. This study aims to examine the impact of geography on physical and psychosocial function after burn injury.
METHODS: Data from the Burn Model Systems National Database (1997-2015) were analyzed. Individuals 18 years and older who were alive at discharge were included. Physical and psychosocial functions were assessed at 6, 12, and 24 months postinjury using the following patient-reported outcome measures: Community Integration Questionnaire, Physical Composite Scale and Mental Composite Scale of the 12-Item Short Form Health Survey, Satisfaction with Appearance Scale, and Satisfaction with Life Scale. Descriptive statistics were generated for demographic and medical data, and mixed regression models were used to assess the impact of geography on long-term outcomes.
RESULTS: The study included 469 burn survivors from the Centers for Medicare and Medicaid Services regions 10, 31 from region 8, 477 from region 6, 267 from region 3, and 41 from region 1. Participants differed significantly by region in terms of race/ethnicity, burn size, burn etiology, and acute care length of stay (P < 0.001). In adjusted mixed model regression analyses, scores of all 5 evaluated outcome measures were found to differ significantly by region (P < 0.05).
CONCLUSIONS: Several long-term physical and psychosocial outcomes of burn survivors vary significantly by region. This variation is not completely explained by differences in population characteristics. Understanding these geographical differences may improve care for burn survivors and inform future policy and resource allocation.
PMID:32040001 | PMC:PMC8265767 | DOI:10.1097/SAP.0000000000002287
J Burn Care Res. 2020 May 2;41(3):640-646. doi: 10.1093/jbcr/iraa011.
ABSTRACT
The Young Adult Burn Outcome Questionnaire (YABOQ) is a validated, English-language patient-reported outcome assessment of young adults' recovery from burn injury across 15 scale domains. We evaluated the cross-cultural validity of a newly developed Spanish version of the YABOQ. Secondary data from English- and Spanish-speaking burn survivors (17 to 30 years of age) were obtained from the Multicenter Benchmarking Study. We conducted classic psychometric analyses and evaluated the measurement equivalence of the English and Spanish YABOQs in logistic and ordinal logistic regression differential item functioning analyses. All multi-item scales in the Spanish YABOQ demonstrated adequate reliability except the Pain and Itch scales. One item in the Perceived Appearance scale showed differential item functioning across English- and Spanish-speaking burn survivors, but the observed differential item functioning had no clinically significant impact on scale-level Perceived Appearance scores. Our findings support the cross-cultural validity of the YABOQ Physical Function, Perceived Appearance, Sexual Function, Emotion, Family Function, Family Concern, Satisfaction with Symptom Relief, Satisfaction with Role, Work Reintegration and Religion scales among English- and Spanish-speaking young adult burn survivors. This work supports the use of these English and Spanish YABOQ scales to assess the effect of therapeutic interventions on young adults' burn outcomes in pooled analyses and to assess disparities in young adults' burn outcomes across language groups.
PMID:31930334 | PMC:PMC9834989 | DOI:10.1093/jbcr/iraa011
Burns. 2020 May;46(3):745-747. doi: 10.1016/j.burns.2019.12.016. Epub 2019 Dec 31.
ABSTRACT
Burn survivors who misuse alcohol and/other substances have been associated with poorer long-term outcomes and clinical complications following injury. The self-reported CAGE questionnaire (Cut down, Annoyed, Guilty, and Eye-opener) is an outcomes assessment tool used to screen for potential substance misuse. Understanding the persistence and emergence of potential substance misuse through examination of CAGE scores may provide important information about this population. Using data collected from the Burn Model System National Database, demographic and clinical characteristics of individuals who reported positive CAGE scores (total score of ≥2) and those who reported negative CAGE scores (total score of 0 or 1) for either alcohol or other drugs were compared.
PMID:31901407 | PMC:PMC9201553 | DOI:10.1016/j.burns.2019.12.016
Am J Phys Med Rehabil. 2020 Jul;99(7):602-607. doi: 10.1097/PHM.0000000000001378.
ABSTRACT
OBJECTIVES: The aim of this study was to examine potential racial/ethnic disparities in community integration for the 2 yrs after burn injury.
DESIGN: A sample of 1773 adults with burn injury from the Burn Model Systems database was used with data on community integration collected at discharge (preinjury recall), 6, 12, and 24 mos after discharge.
METHODS: Four sets of hierarchal linear models determined the most appropriate model for understanding racial/ethnic differences in Community Integration Questionnaire trajectories over time.
RESULTS: Data indicated a decrease in community integration between discharge and 6 mos, a slight increase between 6 mos and 1 yr, and then a plateau between 1 and 2 yrs. White individuals had higher community integration score trajectories over time than black (b = 0.53, P < 0.001) and Hispanic (b = 0.58, P < 0.001) individuals, and community integration scores were similar between black and Hispanic individuals (b = -0.05, P = 0.788). These racial/ethnic disparities remained after accounting for age, sex, total burned surface area, number of days in rehabilitation, and active range of motion deficits.
CONCLUSIONS: Additional rehabilitation resources should be targeted to helping black and Hispanic individuals integrate back into their communities after burn injury.
PMID:31876543 | PMC:PMC8265766 | DOI:10.1097/PHM.0000000000001378
J Burn Care Res. 2020 Feb 19;41(2):270-279. doi: 10.1093/jbcr/irz186.
ABSTRACT
Participant attrition in longitudinal studies can lead to substantial bias in study results, especially when attrition is nonrandom. A previous study of the Burn Model System (BMS) database prior to 2002 identified participant and study-related factors related to attrition. The purpose of the current study was to examine changes in attrition rates in the BMS longitudinal database since 2002 and to revisit factors associated with attrition. Individuals 18 years and older enrolled in the BMS database between 2002 and 2018 were included in this study. Stepwise logistic regression models identified factors significantly associated with attrition at 6, 12, and 24 months postburn injury. The percentage of individuals lost to follow-up was 26% at 6 months, 33% at 12 months, and 42% at 24 months. Factors associated with increased risk of loss to follow-up across two or more time points include male sex, lower TBSA burn size, being unemployed at the time of burn, shorter duration of acute hospital stay, younger age, not having private health insurance or workers' compensation, and a history of drug abuse. Retention levels in the BMS have improved by at least 10% at all time points since 2002. The BMS and other longitudinal burn research projects can use these results to identify individuals at high risk for attrition who may require additional retention efforts. Results also indicate potential sources of bias in research projects utilizing the BMS database.
PMID:31738436 | PMC:PMC9121819 | DOI:10.1093/jbcr/irz186
Arch Phys Med Rehabil. 2019 Nov 13:S0003-9993(19)31369-3. doi: 10.1016/j.apmr.2019.11.003. Online ahead of print.
ABSTRACT
A special supplement to the Archives of Physical Medicine and Rehabilitation in 2007 reported selected findings of research from the first 13 years of the BMS Centers and Database Coordinating Center. This special supplement is the second such effort and reports on the growth of the BMS National Longitudinal Database (BMS NDB) since that time and select new research findings from the BMS centers.
PMID:31733193 | DOI:10.1016/j.apmr.2019.11.003
Burns. 2020 Feb;46(1):17-18. doi: 10.1016/j.burns.2019.10.023. Epub 2019 Nov 13.
NO ABSTRACT
PMID:31732219 | PMC:PMC9221643 | DOI:10.1016/j.burns.2019.10.023
J Burn Care Res. 2020 Feb 19;41(2):377-383. doi: 10.1093/jbcr/irz185.
ABSTRACT
While disparities in healthcare outcomes and services for vulnerable populations have been documented, the extent to which vulnerable burn populations demonstrate disparities in long-term care is relatively underexplored. This study's goal was to assess for differences in long-term occupational or physical therapy (OT/PT) and psychological service use after burn injury in vulnerable populations. Data from the Burn Model System National Database (2006-2015) were analyzed. The vulnerable group included participants in one or more of these categories: 65 years of age or older, nonwhite, no insurance or Medicaid insurance, preinjury receipt of psychological therapy or counseling, preinjury alcohol and/or drug misuse, or with a preexisting disability. Primary outcomes investigated were receipt of OT/PT and psychological services. Secondary outcomes included nine OT/PT subcategories. Outcomes were examined at 6, 12, and 24 months postinjury. One thousand one hundred thirty-six burn survivors (692 vulnerable; 444 nonvulnerable) were included. The vulnerable group was mostly female, unemployed at time of injury, and with smaller burns. Both groups received similar OT/PT and psychological services at all time points. Adjusted regression analyses found that while the groups received similar amounts services, some vulnerable subgroups received significantly more services. Participants 65 years of age or older, who received psychological therapy or counseling prior to injury, and with a preexisting disability received more OT/PT and psychological or peer support services at follow-up. Overall, vulnerable and nonvulnerable groups received comparable OT/PT and psychological services. The importance of long-term care among vulnerable subgroups of the burn population is highlighted by this study. Future work is needed to determine adequate levels of follow-up services.
PMID:31710682 | PMC:PMC9306190 | DOI:10.1093/jbcr/irz185
Burns. 2019 Dec;45(8):1775-1782. doi: 10.1016/j.burns.2019.02.014. Epub 2019 Nov 2.
ABSTRACT
To determine the association between potential risk factors and multiple organ failure (MOF) in severe burn adult patients, we performed a secondary analysis of data from the "Inflammation and the Host Response to Injury" database, which included patients from six burn centers in the United States between 2003 and 2009. Three hundred twenty-two adult patients (aged ≥16 years) with severe burns (≥20.0% total body surface area [TBSA]) were included. MOF was defined according to the Denver score. Potential risk factors were analyzed for their association with MOF. Models were built using multivariable logistic regression analysis. Eighty-eight patients (27.3%) developed MOF during the study period. We found that TBSA, age, and inhalation injury were significant risk factors for MOF. This predictive model showed good performance, with the total area under the receiver operating characteristic curve being 0.823. Moreover, among patients who developed MOF, inhalation injury was significantly associated with the development of MOF in the acute phase (within three days of injury) (adjusted odds ratio 3.1; 95% confidence interval 1.1-8.3). TBSA, age, lactate, and Denver score within 24h were associated with the late phase development of MOF. Thus, we have identified key risk factors for the onset of MOF after severe burn injury. Our findings contribute to the understanding of individualized treatment and will potentially allow for efficient allocation of resources and a lower threshold for admission to an intensive care unit, which can prevent the development of MOF and eventually reduce mortality.
PMID:31690472 | DOI:10.1016/j.burns.2019.02.014
Burns. 2020 May;46(3):531-538. doi: 10.1016/j.burns.2019.09.003. Epub 2019 Oct 20.
ABSTRACT
INTRODUCTION: Self-inflicted burn (SIB) injuries are relatively rare, but patients may experience complex biopsychosocial challenges. This study aimed to compare long-term physical and psychological outcomes for individuals with SIB and non-SIB injuries.
METHODS: Records of adult SIB (n = 125) and non-SIB (n = 3604) injuries were collected from U.S. burn centers within the Burn Model System between 1993 and 2018. Assessments were administered at discharge, 6 months, 24 months, 5 years, and 10 years.
RESULTS: SIB patients were more often younger, unmarried, unemployed, male, struggling with pre-morbid psychiatric issues, and injured by fire/flame (all p < 0.001). SIB injury predicted prolonged mechanical ventilation, hospitalization, and rehabilitation (all p < 0.001). After injury, SIB patients had increased anxiety at 24 months (p = 0.0294), increased suicidal ideation at 5 years (p = 0.004), and clinically worse depression at 10 years (p = 0.0695). SIB patients had increased mortality across 24 months compared to non-SIB patients (OR = 4.706, p = 0.010).
CONCLUSION: SIB injuries are associated with worse physical and psychological outcomes compared to non-SIB injuries including complicated hospitalizations and chronic problems with anxiety, depression, suicidality, and mortality, even when controlling for common indicators of severity such as burn size. This underscores the importance of multidisciplinary treatment, including mental healthcare, and long-term follow-up for SIB patients. Identified pre-morbid risk factors indicate the need for targeted injury prevention.
PMID:31640886 | DOI:10.1016/j.burns.2019.09.003
Arch Phys Med Rehabil. 2020 Jan;101(1S):S71-S85. doi: 10.1016/j.apmr.2019.09.009. Epub 2019 Oct 15.
ABSTRACT
OBJECTIVE: To investigate the effect of patient and injury characteristics on employment for working-age, adult survivors of burn injury using the multicenter Burn Model System national database.
DESIGN: Longitudinal survey.
SETTING: Multicenter regional burn centers.
PARTICIPANTS: Adult burn survivors (N=967) age≥18 years with known employment status prior to injury were included in the analysis at 12 months after injury.
INTERVENTIONS: Not applicable.
MAIN OUTCOME MEASURES: Employment status at 12 months after injury.
RESULTS: The analyses determined that those employed preinjury had higher odds of being employed (odds ratio [OR]=8.1; 95% confidence interval [CI], 4.9-13.1). White, non-Hispanic individuals were also more likely to be employed (OR=1.49; 95% CI, 1.0-2.1). Older individuals, females, those with longer hospitalizations, amputation during the acute hospitalization, and those with high pain interference at hospital discharge had lower odds of working after injury. Preinjury living situation, preinjury alcohol and drug misuse, number of acute operations and burn size (total body surface area, %) were not significant predictors of employment status at 12 months after burn injury.
CONCLUSION: Preinjury employment remains the most significant predictor for postburn employment. Although past reports have focused on predictors for postburn employment, we believe that we need to seek greater understanding of modifiable risk factors for unemployment and examine issues related to work retention, performance, accommodations, and career trajectories for the working-age survivor of burn injury.
PMID:31626744 | DOI:10.1016/j.apmr.2019.09.009
J Burn Care Res. 2020 May 2;41(3):503-534. doi: 10.1093/jbcr/irz150.
ABSTRACT
The objective of this review was to systematically evaluate the available literature addressing the use of orthoses (splints and casts) with adult and pediatric burn survivors and determine whether practice guidelines could be proposed. This review provides evidence-based recommendations specifically for rehabilitation professionals who are responsible for burn survivor rehabilitation. A summary recommendation was made after the literature was retrieved using a systematic review and critical appraisal by multiple authors. The level of evidence of the literature was determined in accordance with the Oxford Centre for Evidence-based Medicine criteria. Due to the low level of evidence in the available literature, only one practice guideline could be recommended: orthotic use should be considered as a treatment choice for improving range of motion or reducing contracture in adults who have sustained a burn injury. To address the rehabilitation-specific gaps found in the literature regarding orthotic use in burn rehabilitation and provide guidance to clinicians, a formal expert consensus exercise was conducted as a final step to the project. The resultant manuscript provides a summary of the literature regarding orthotic use with burn patients, one practice guideline, proposed orthotic terminology and additional practice recommendations based on expert opinion. The limitations in the current literature are also discussed, and suggestions are made for future studies in the area of orthotic use after burn injury.
PMID:31504622 | DOI:10.1093/jbcr/irz150
Am J Phys Med Rehabil. 2020 Jan;99(1):1-6. doi: 10.1097/PHM.0000000000001266.
ABSTRACT
OBJECTIVE: The aim of the study was to determine the impact of weekend versus weekday admission to an inpatient rehabilitation facility on the risk of acute care transfer in patients with stroke.
DESIGN: This was a retrospective analysis using the Uniform Data System for Medical Rehabilitation, a national database comprising data from 70% of US inpatient rehabilitation facilities. A total of 1,051,436 adult (age ≥18 yrs) stroke cases were identified between 2002 and 2014 that met inclusion criteria. Logistic regression models were developed to test for associations between weekend (Friday-Sunday) versus weekday (Monday-Thursday) inpatient rehabilitation facility admission and transfer to acute care (primary outcome) and inpatient rehabilitation facility length of stay (secondary outcome), adjusting for relevant patient, medical, and facility variables. A secondary analysis examined acute care transfer from 2002 to 2009 before passage of the Affordable Care Act (ACA), 2010 to 2012 post-Affordable Care Act, and 2013 to 2014 after implementation of the Hospital Readmissions Reduction Program.
RESULTS: Weekend inpatient rehabilitation facility admission was associated with increased odds of acute care transfer (odds ratio = 1.06, 95% confidence interval = 1.04-1.08) and slightly shorter inpatient rehabilitation facility length of stay (P < 0.001). Overall, the risk of acute care transfer decreased after the ACA and Hospital Readmissions Reduction Program.
CONCLUSIONS: Weekend admission to inpatient rehabilitation facility may pose a modest increase in the risk of transfer to acute care in patients with stroke.
TO CLAIM CME CREDITS: Complete the self-assessment activity and evaluation online at http://www.physiatry.org/JournalCME CME OBJECTIVES: Upon completion of this article, the reader should be able to: (1) Understand disparities in obesity rates among adolescents with mobility disabilities; (2) Describe limitations of current clinical screening methods of obesity in children with mobility disabilities; and (3) Identify potential alternatives for obesity screening in children with mobility disabilities.
LEVEL: Advanced ACCREDITATION: The Association of Academic Physiatrists is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.The Association of Academic Physiatrists designates this Journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
PMID:31335342 | PMC:PMC6920532 | DOI:10.1097/PHM.0000000000001266
PM R. 2020 Mar;12(3):324-326. doi: 10.1002/pmrj.12220. Epub 2019 Sep 12.
NO ABSTRACT
PMID:31325349 | DOI:10.1002/pmrj.12220
Arch Phys Med Rehabil. 2019 Nov;100(11):2015-2021. doi: 10.1016/j.apmr.2019.06.007. Epub 2019 Jul 3.
ABSTRACT
OBJECTIVE: To examine differences in long-term employment outcomes in the postacute care setting.
DESIGN: Retrospective review of the prospectively collected Burn Model System National Database.
SETTING AND PARTICIPANTS: A total of 695 adult survivors of burn injury enrolled between May 1994 and June 2016 who required postacute care at a Burn Model System center following acute care discharge were included. Participants were divided into 2 groups based on acute care discharge disposition. Those who received postacute care at an inpatient rehabilitation facility (IRF) following acute care were included in the IRF group (N=447), and those who were treated at a skilled nursing facility, long-term care hospital, or other extended-care facility following acute care were included in the Other Rehab group (N=248).
INTERVENTIONS: Not applicable.
MAIN OUTCOME MEASURES: Employment status at 12 months postinjury. Propensity score matching and logistic regression were utilized to determine the effect of postacute care setting on employment status.
RESULTS: Individuals in the IRF group had larger burns and were more likely to have an inhalation injury and to undergo amputation. At 12 months postinjury, the IRF group had over 9 times increased odds of being employed compared to the Other Rehab group, using propensity score matching (P=.046).
CONCLUSIONS: While admitting patients with more severe injuries, IRFs provided a long-term benefit for survivors of burn injury in terms of regaining employment. Given the current lack of evidence-based guidelines on postacute care decisions, the results of this study shed light on the potential benefits of the intensive services provided at IRFs in this population.
PMID:31278926 | PMC:PMC9201557 | DOI:10.1016/j.apmr.2019.06.007
J Burn Care Res. 2020 Jan 30;41(1):84-94. doi: 10.1093/jbcr/irz110.
ABSTRACT
Due to the rapid developmental growth in preschool-aged children, more precise measurement of the effects of burns on child health outcomes is needed. Expanding upon the Shriners Hospitals for Children/American Burn Association Burn Outcome Questionnaire 0 to 5 (BOQ0-5), we developed a conceptual framework describing domains important in assessing recovery from burn injury among preschool-aged children (1-5 years). We developed a working conceptual framework based on the BOQ0-5, the National Research Council and Institute of Medicine's Model of Child Health, and the World Health Organization's International Classification of Functioning, Disability, and Health for Children and Youth. We iteratively refined our framework based on a literature review, focus groups, interviews, and expert consensus meetings. Data were qualitatively analyzed using methods informed by grounded theory. We reviewed 95 pediatric assessments, conducted two clinician focus groups and six parent interviews, and consulted with 23 clinician experts. Three child health outcome domains emerged from our analysis: symptoms, functioning, and family. The symptoms domain describes parents' perceptions of their child's pain, skin-related discomfort, and fatigue. The functioning domain describes children's physical functioning (gross and fine motor function), psychological functioning (internalizing, externalizing, and dysregulation behavior; trauma; toileting; resilience), communication and language development (receiving and producing meaning), and social functioning (connecting with family/peers, friendships, and play). The family domain describes family psychological and routine functioning outcomes.
PMID:31222201 | PMC:PMC9306191 | DOI:10.1093/jbcr/irz110
J Burn Care Res. 2019 Oct 16;40(6):776-784. doi: 10.1093/jbcr/irz082.
ABSTRACT
The Burn Outcomes Questionnaire for children ages 5-18 years (BOQ5-18) is a widely used, reliable, and valid parent-reported outcome measure designed to assess children's recovery from burn injuries in 12 physical and psychosocial domains. This study evaluated the feasibility, acceptability, and usefulness of a feedback system that delivered BOQ and Pediatric Symptom Checklist (PSC-17; a widely used measure of psychosocial functioning) results to burn care clinicians prior to an outpatient appointment or a postoperative surgical encounter. The BOQ and the PSC-17 were administered to the parents of 147 children receiving outpatient or surgical care in two pediatric burn hospitals. Clinician and parent perceptions of the feedback system were evaluated using debriefing questionnaires. Over half of all patients were at-risk on at least one BOQ subscale, and risk on three or more BOQ domains was significantly associated with a higher likelihood of poor psychological scores on the PSC-17 (P < .001). Significant differences in BOQ scores were found between the two hospital sites on four BOQ subscales, three related to physical ability and one to psychosocial well-being. Parent ratings of the feedback system were positive, with 90% of parents in both settings agreeing that the BOQ tablet experience was easy and helpful. Clinician attitudes differed across the two settings with more positive clinician ratings of the system in the outpatient setting (P < .001). Clinician interviews revealed that the data was especially useful in bringing to light psychosocial aspects of functioning relevant to long-term recovery from burn injuries.
PMID:31102446 | DOI:10.1093/jbcr/irz082
J Burn Care Res. 2019 Oct 16;40(6):792-795. doi: 10.1093/jbcr/irz084.
ABSTRACT
Long-term trials are key to understanding chronic symptoms such as pain and itch. However, challenges such as high attrition rates and poor recruitment are common when conducting research. The aim of this work was to explore these issues within a long-term randomized control trial using transcranial direct current stimulation to treat pain and itch. This parallel double blinded, placebo-controlled randomized trial was comprised of 15 transcranial direct current stimulation visits and 7 follow-up visits. Participants were over the age of 18, had a burn injury that occurred at least 3 weeks before enrollment, and reported having pain and/or itch that was moderate to severe in intensity. A total of 31 subjects were randomized into either an active or sham transcranial direct current stimulation groups. There were no significant differences between the groups in terms of age, race, education, baseline depression, or anxiety. The median dropout time was at visit 19 (visit 16 [SE = 1.98] for the sham group and visit 19 [SE = 1.98] for the active group). Analysis showed no differences in the dropout rate between groups [χ2(1) = 0.003, P = .954]. The dropout rate was 46.7% for the sham group and 43.8% for the active group. Overall, 45.2% of the subjects dropped out of the trial. Long-term clinical trials are an essential part of evaluating interventions for symptoms such as chronic pain and itch. However, as seen in this trial, long-term studies in the burn population often face recruitment and adherence challenges.
PMID:31102438 | DOI:10.1093/jbcr/irz084
J Burn Care Res. 2019 Aug 14;40(5):669-677. doi: 10.1093/jbcr/irz076.
ABSTRACT
INTRODUCTION: Work integration and retention after burn injury is a key outcome. Little is known about how burn survivors reintegrate into the workplace. This article compares scores on the Life Impact Burn Recovery Evaluation (LIBRE) Profile, a burn-specific measure of social participation, between burn survivors and general population samples, focusing on the Work and Employment domain.
METHODS: Convenience samples of burn survivors and the U.S. population were obtained. Differences in demographic and clinical characteristics and LIBRE Profile scores were assessed. To examine work and employment, we compared family and friends, social activities, and social interactions scores among working vs nonworking burn survivors.
RESULTS: Six hundred and one burn survivors (320 employed) and 2000 U.S. residents (1101 employed) were surveyed. The mean age (P = .06), distributions of sex (P = .35), and Hispanic ethnicity (P = .07) did not differ significantly. Distributions of race (P < .01) and education (P = .01) differed significantly. The burn survivor sample had higher scores, demonstrating higher participation, for work and employment (mean = 49.5, SD = 9.42) than the general sample (mean = 46.94, SD = 8.94; P < .0001), which persisted after adjusting for demographic characteristics. Scores on the three domains administered to all respondents were higher (P < .001) for working than nonworking burn survivors.
CONCLUSION: Distributions indicated higher social participation in the burn survivor sample than the general sample. Possible explanations include sample bias; resilience, posttraumatic growth, or response-shift of survivors; and limitations of using items in the general sample. Working burn survivors scored higher than those not working. Future work can explore factors that mediate higher scores and develop interventions.
PMID:31069384 | PMC:PMC9302902 | DOI:10.1093/jbcr/irz076
J Burn Care Res. 2019 Aug 14;40(5):696-702. doi: 10.1093/jbcr/irz074.
ABSTRACT
Social and emotional recovery from burn injury is a complex process impacted by both clinical and social factors. Because level of education (LOE) has been correlated to overall health, health outcomes, and life expectancy, we questioned whether LOE might be associated with successful social recovery after burn injury. The Life Impact Burn Recovery Evaluation (LIBRE) data set served as a novel tool to explore this question. The LIBRE project is a collaborative effort designed to provide a clinical yardstick for social reintegration among burn survivors. After institutional review board approval, 601 burn survivor respondents, aged 18 or over with >5% TBSA burn were surveyed and a six-scale, 126-item LIBRE Profile was derived from their responses. LOE was collapsed into four categories ranging from less than high school equivalency certificate to graduate degree. Impact of burn injury on subsequent LOE was examined by splitting the sample into those burned at age 30 years or less and those burned at greater than 30 years of age. Regression models were run to estimate associations between education and scale scores with adjustment for age at injury, sex, marital status, work status, TBSA, and time since burn. Regression models were run on the entire cohort and then stratified by age at burn injury (≤30 vs >30). Among all subjects, we found an association between LOE and social recovery as measured by LIBRE scale scores. This association was contributed entirely from the cohort burned at age 30 or less: for those burned at greater than age 30, there was no association between LOE and social recovery. Of particular interest, the distribution of LOE among those burned at ≤ 30 was very similar to LOE distribution in both millennials and in the U.S. population at large. LOE appears to be associated with social recovery for those burned at younger ages but not for those burned at over age 30. More importantly, burn injury during schooling may have no impact on a survivor's educational trajectory since distribution of LOE in our ≤30 cohort mirrors that of the general population. LOE and age at burn injury may provide a quick screen for survivors at risk of difficult social reintegration, allowing providers to target those at risk with additional peer support and counseling.
PMID:31067572 | PMC:PMC10108574 | DOI:10.1093/jbcr/irz074
PLoS One. 2019 May 6;14(5):e0215898. doi: 10.1371/journal.pone.0215898. eCollection 2019.
ABSTRACT
This paper explores extreme response class to the Life Impact Burn Recovery Evaluation (LIBRE) Profile, a measure of social participation in burn survivors. We fit a Multidimensional Generalized Partial Credit Model (MGPCM) with a positive extreme response class (PERS) factor and compared this model with the original MGPCM, estimated the impact that PERS has on scores, and examined the personal characteristics that may result in an individual more likely to respond in a fashion that would inflate their true low scores. The average impact of the PERS, based upon the root mean squared bias, ranged from 0.27 to 0.50 of a standard deviation of the scale. Individuals who were older, had participated in a burn survivor support group, and had selected to self-administer the measure were less likely to have a high PERS bias that masks low scores. Future work can consider PERS when measuring the psychosocial impacts of burn injuries and other health conditions.
PMID:31059527 | PMC:PMC6502351 | DOI:10.1371/journal.pone.0215898
J Burn Care Res. 2019 Jun 21;40(4):398-405. doi: 10.1093/jbcr/irz063.
ABSTRACT
Oxandrolone, a testosterone analog, is used to counteract the catabolic effects of burn injury. Recent animal studies suggest a possible hormonal association with heterotopic ossification (HO) development postburn. This work examines oxandrolone administration and HO development by exploring historical clinical data bridging the introduction of oxandrolone into clinical practice. Additionally, we examine associations between oxandrolone administration and HO in a standardized mouse model of burn/trauma-related HO. Acutely burned adults admitted between 2000 and 2014, survived through discharge, and had a HO risk factor of 7 or higher were selected for analysis from a single burn center. Oxandrolone administration, clinical and demographic data, and elbow HO were recorded and were analyzed with logistic regression. Associations of oxandrolone with HO were examined in a mouse model. Mice were administered oxandrolone or vehicle control following burn/tenotomy to examine any potential effect of oxandrolone on HO and were analyzed by Student's t test. Subjects who received oxandrolone had a higher incidence of elbow HO than those that did not receive oxandrolone. However, when controlling for oxandrolone administration, oxandrolone duration, postburn day oxandrolone initiation, HO risk score category, age, sex, race, burn size, and year of injury, there was no significant difference between rates of elbow HO between the two populations. In agreement with the review, in the mouse model, while there was a trend toward the oxandrolone group developing a greater volume of HO, this did not reach statistical significance.
PMID:31053861 | PMC:PMC6587410 | DOI:10.1093/jbcr/irz063
Arch Phys Med Rehabil. 2019 May;100(5):891-898. doi: 10.1016/j.apmr.2018.10.004. Epub 2018 Oct 26.
ABSTRACT
OBJECTIVE: Common data elements (CDEs) promote data sharing, standardization, and uniform data collection, which facilitate meta-analyses and comparisons of studies. Currently, there is no set of CDEs for all trauma populations, but their creation would allow researchers to leverage existing databases to maximize research on trauma outcomes. The purpose of this study is to assess the extent of common data collection among 5 trauma databases.
DESIGN: The data dictionaries of 5 trauma databases were examined to determine the extent of common data collection. Databases included 2 acute care databases (American Burn Association's National Burn Data Standard and American College of Surgeons' National Trauma Data Standard) and 3 longitudinal trauma databases (Burn, Traumatic Brain Injury, Spinal Cord Injury Model System National Databases). Data elements and data values were compared across the databases. Quantitative and qualitative variations in the data were identified to highlight meaningful differences between datasets.
SETTING: N/A.
PARTICIPANTS: N/A.
INTERVENTIONS: N/A.
MAIN OUTCOME MEASURES: N/A.
RESULTS: Of the 30 data elements examined, 14 (47%) were present in all 5 databases. Another 9 (30%) elements were present in 4 of the 5 databases. The number of elements present in each database ranged from 23 (77%) to 26 (86%). There were inconsistencies in the data values across the databases. Twelve of the 14 data elements present in all 5 databases exhibited differences in data values.
CONCLUSIONS: This study demonstrates inconsistencies in the documentation of data elements in 5 common trauma databases. These discrepancies are a barrier to database harmonization and to maximizing the use of these databases through linking, pooling, and comparing data. A collaborative effort is required to develop a standardized set of elements for trauma research.
PMID:31030731 | PMC:PMC9140315 | DOI:10.1016/j.apmr.2018.10.004
J Neurotrauma. 2019 Sep 1;36(17):2513-2520. doi: 10.1089/neu.2018.6014. Epub 2019 May 16.
ABSTRACT
Initial studies examining patient demographics and outcomes in traumatic brain injury (TBI) suggest a trend toward increasing patient age and decreasing rehabilitation length of stay, but such studies have not been repeated since the passage of healthcare reform legislation, most notably the Affordable Care Act. This study utilized the Uniform Data System for Medical Rehabilitation® (UDSMR) for patients admitted to medical rehabilitation facilities after sustaining a TBI from January 1, 2002 through December 31, 2016. Trends for demographic and medical data were evaluated. In total, 233,843 patients from 1290 facilities were included; mean patient age increased from 54.1 to 64.8 years, rehabilitation length of stay decreased from 19 to 14.5 days, and mean admission Functional Independence Measure® (FIM) decreased from 56.9 to 54.5. Sex and racial distribution remained relatively stable across all years, as did discharge FIM. There was an increase in Medicare patients from 40.7% to 62.1%, a concomitant decrease in commercially insured patients from 29.2% to 15.4%, and a decrease in unreimbursed patients from 7.2% to 2.6% over the course of the study. Based on these data, medical rehabilitation facilities appear to be admitting an older TBI patient population that is less functional on admission and discharging them after shorter rehabilitation lengths of stay. Similar discharge functional status, despite shorter rehabilitation lengths of stay and an older population may suggest a change in the typical mechanism of injury. Many current TBI patients would fail to meet inclusion criteria for post-acute clinical trials in TBI because of their age, and treatments based on such trials may not be generalizable, which has significant implications on both research and clinical care realms within brain injury rehabilitation.
PMID:30887892 | DOI:10.1089/neu.2018.6014
Instruments, Tools, & Guidelines
Burn Outcome Questionnaires (BOQs)
BOQs are patient- and family-reported outcome metrics for children of all ages. The questionnaires are broken up into several categories:
- ages 0-4
- ages 5-18
- ages 18-30 (young adult BOQ)
Heterotopic Ossification Risk Scoring System
Heterotopic Ossification is a rare but severely debilitating complication of burn injuries. We developed a risk scoring system that can be used to predict heterotopic ossification at the time of admission to the hospital.
Guidelines for Burn Care Under Austere Conditions
A series of articles was authored by members of the American Burn Association dedicated to disaster preparedness. These articles specifically address how to carry on effective burn care following a mass casualty event.